Therapie & Praxis
Interprofessional outpatient rehabilitation
Discover how Ambulant-Physio Ergo Logo in Cottbus blends physiotherapy, occupational therapy, speech therapy, and robotics to provide evidence-based, participation-oriented care. Learn more about their interdisciplinary concept and inspiring patient outcomes.

An interview with Torsten Erler from Ambulant‑Physio Ergo Logo GmbH in Cottbus.
Ambulant-Physio Ergo Logo GmbH in Cottbus is an interdisciplinary centre for occupational therapy, physiotherapy and speech therapy. A competence centre for perception, movement and communication. In addition to the therapeutic specialist groups, social education is also an important link in the holistic care concept. All interventions are client-centred and focused on enabling social participation. To achieve agreed rehabilitation goals, the interdisciplinary treatment team relies on a useful combination of empirical rehabilitation concepts with the latest innovations. In this interview, Torsten Erler, founder and owner of Ambulant-Physio Ergo Logo Cottbus, explains how the desire for mobility, self-care, communication and an individual lifestyle is the starting point for interdisciplinary cooperation and what role modern technologies, such as robotics, play in everyday treatment.
If we are able to reflect critically on our actions within the practice and can make this part of our self-image as practitioners – whatever the discipline – then we will be able to provide participation-oriented therapy.
Interviewer: Mr Erler, thank you very much for the interview. How would you describe in a few sentences what you have created in your therapy centre in Cottbus?
Torsten Erler: We combine tradition with innovation. We have been gaining extensive experience with the major empirical treatment concepts for 25 years and at the same time we see the need for evidence-based, guideline-oriented practice. We are innovative and we work with the latest technologies. One challenge is that we specialise in out-of-hospital intensive care, among other things. I’m sure we’ll talk about this later, but this already explains why we use a healthy mix of tradition and modernity.
Interviewer: We’ll go into that in more detail later. Let’s first talk about interprofessionality. You combine physiotherapy, occupational therapy and speech therapy. The practice landscape in Germany today is predominantly organised on a unidisciplinary basis. What is the benefit of patients receiving all their therapies at the same location?
Torsten Erler: As I mentioned, many of our patients have serious conditions. Some of them have a tracheostomy tube and a stomach tube for artificial feeding since they can’t swallow. All of this places special demands on therapy that cannot be met by one speciality alone. Our advantage is that we can work together in an interdisciplinary way. This not only increases the duration of treatment, but also the quality of care, and opens up completely new treatment options.
Interviewer: What role do the relatives of seriously affected patients play?
Torsten Erler: Particularly in the case of patients with impaired consciousness and cognitive limitations, the relatives are involved whenever possible – if they want to be – and play an active role in shaping the therapy. Relatives can often interpret the patient’s behaviour during therapy in a completely different way than we can. The assessment of facial expressions, gestures and other physical reactions is extremely important. And who can do this better than those closest to the patients? We want to put our patients at the very centre of treatment. This is only possible in the case of patients with serious conditions if there is close co-ordination and co-operation with the relatives, nursing staff and physicians. From goal setting to the continuous therapy process itself, we are connected as well as we can be with every actor involved in the overall care process.
Interviewer: On your website, you write that Ambulant-Physio Ergo Logo is the right choice for all those looking for good therapy. What makes for good therapy in your opinion, Mr Erler?
Torsten Erler: We combine tradition with innovation. We have been gaining extensive experience with the major empirical treatment concepts for 25 years and at the same time we see the need for evidence-based, guideline-oriented practice. We are innovative and we work with the latest technologies. One challenge is that we specialise in out-of-hospital intensive care, among other things. I’m sure we’ll talk about this later, but this already explains why we use a healthy mix of tradition and modernity.
Interviewer: We’ll go into that in more detail later. Let’s first talk about interprofessionality. You combine physiotherapy, occupational therapy and speech therapy. The practice landscape in Germany today is predominantly organised on a unidisciplinary basis. What is the benefit of patients receiving all their therapies at the same location?
Torsten Erler: As I mentioned, many of our patients have serious conditions. Some of them have a tracheostomy tube and a stomach tube for artificial feeding since they can’t swallow. All of this places special demands on therapy that cannot be met by one speciality alone. Our advantage is that we can work together in an interdisciplinary way. This not only increases the duration of treatment, but also the quality of care, and opens up completely new treatment options.
Interviewer: What role do the relatives of seriously affected patients play?
Torsten Erler: Particularly in the case of patients with impaired consciousness and cognitive limitations, the relatives are involved whenever possible – if they want to be – and play an active role in shaping the therapy. Relatives can often interpret the patient’s behaviour during therapy in a completely different way than we can. The assessment of facial expressions, gestures and other physical reactions is extremely important. And who can do this better than those closest to the patients? We want to put our patients at the very centre of treatment. This is only possible in the case of patients with serious conditions if there is close co-ordination and co-operation with the relatives, nursing staff and physicians. From goal setting to the continuous therapy process itself, we are connected as well as we can be with every actor involved in the overall care process.
Interviewer: On your website, you write that Ambulant-Physio Ergo Logo is the right choice for all those looking for good therapy. What makes for good therapy in your opinion, Mr Erler?
Torsten Erler: That’s almost a philosophical questions (laughs). In my opinion, the answer is an in-depth self-examination. Motor skills, cognition and motivation are necessary for the recovery of skills. We often cling to the knowledge of previous successful therapies. But every therapeutic process always requires the therapist to adapt to the client’s situation and to the constantly developing findings on methodology, proof of effect and the usefulness of the therapeutic tool in question. In my professional career, it has often been my experience that the necessary humility of those in charge – in the face of the complex changes to the patient’s body, mind and soul – quickly diminishes. Especially when dealing with the complexity of disorders and the biopsychosocial consequences for our clients, our minds must remain energetic and hungry to learn. A great respect for the client’s endurance and struggle against their own demons should spur us on in the search for the ideal therapy. I’m in no way trying to be provocative. If we are able to reflect critically on our actions within the practice and can make this part of our self-image as practitioners – whatever the discipline – then we can provide good therapy to patients. This is what Ambulant-Physio Ergo Logo stands for as an interdisciplinary team. We are looking for the IDEAL of outpatient rehabilitation. Our interactive training centre will be opening soon.
Interviewer: In terms of modern treatment approaches, you are a strong advocate of device-assisted therapy and the use of robotics in your practice. What are the advantages of this?
Interviewer: In terms of modern treatment approaches, you are a strong advocate of device-assisted therapy and the use of robotics in your practice. What are the advantages of this?
If we didn’t have the equipment, we wouldn’t be able to stand or walk for thirty minutes with our most severely affected patients.
Torsten Erler: I’ll give you an example. We have a patient who is in remission after a vegetative state. The patient has regained the ability to swallow, and the ability to communicate by blinking, but is still fitted with a tracheostomy tube. What we offer patients such as these is a combination therapy consisting of intensive swallowing therapy in conjunction with mobilisation and verticalisation. The idea is to get patients standing and walking to activate the torso and head posture reactions in order to improve swallowing quality. In a way, this is a professional provocation. But we haven’t stopped there, we have gained experience in the clinic and have successfully managed to transfer the idea conceptually to the outpatient setting. For this, we need appropriate technologies and equipment, such as the dynamic standing frame and the electromechanical gait trainer. If we didn’t have the equipment, we wouldn’t be able to stand or walk for thirty minutes with our most severely affected patients. We tried that at the beginning. But failed because of the everyday reality. The patients stood for a short time during the thirty minutes and perhaps took a few steps. After that, it was the therapists who were at their performance limit, rather than the patient (grins).
Interviewer: What exactly are the effects of combining the therapies in this way?
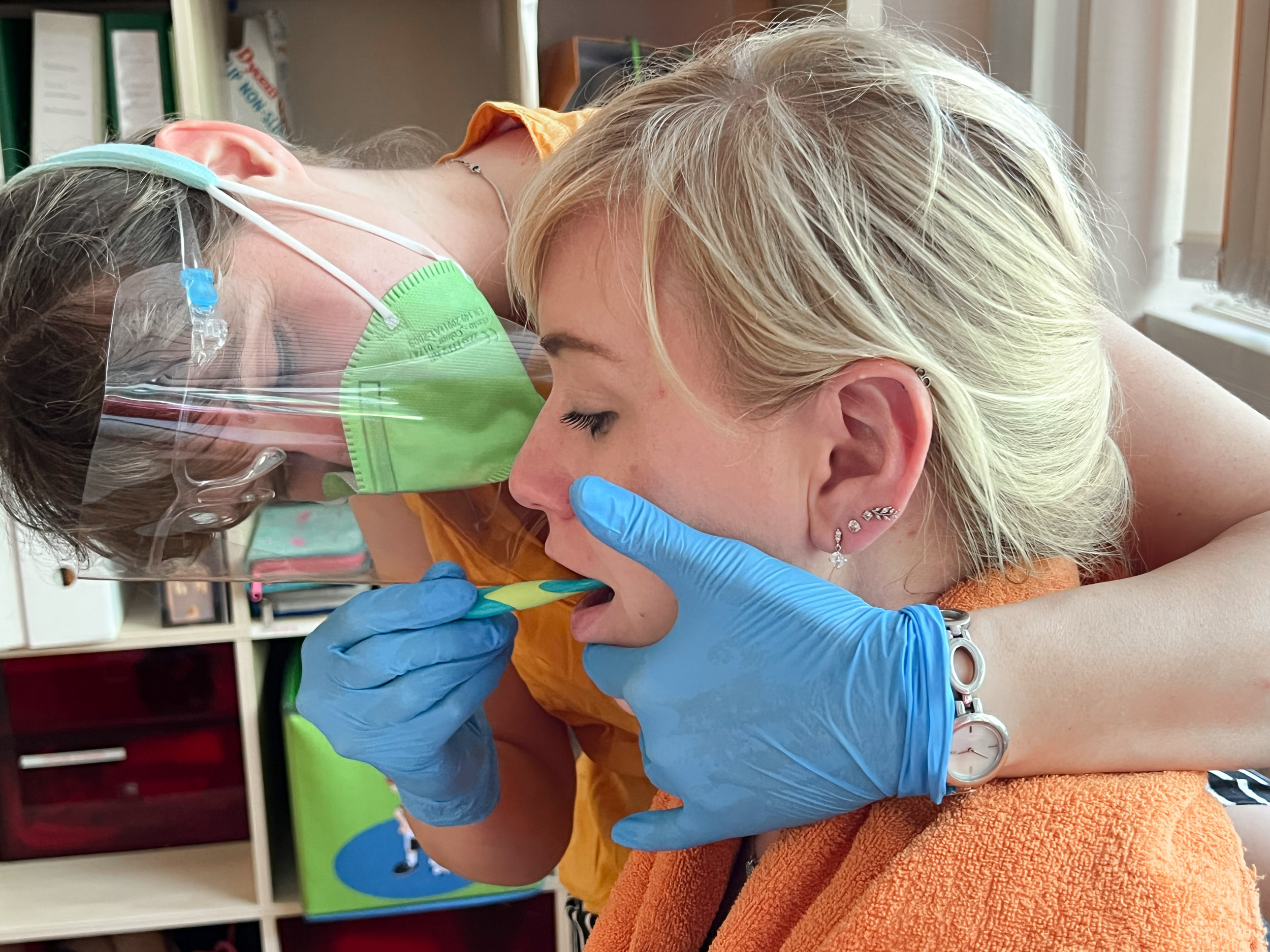
Torsten Erler: We experience a significant increase in patient vigilance. Through verticalisation, we achieve conditions for an ideal alignment of the body with respect to gravity, where the head is first of all positioned and swallowing is physiologically possible. This is also possible when lying down or sitting, but it is often much better when standing. Sometimes we even do gait training, which we interrupt in order to include short swallowing sequences or to do oral stimulation. The device support is simply great. It allows us to work very effectively and efficiently, to make corrections in a few easy steps and create optimal conditions. This is very fortunate and would not be possible without the use of technology.
Interviewer: How do you ensure that the treatments are actually goal-oriented and effective?
Torsten Erler: We have set up our own ICF-based documentation for this purpose. This defines participation and includes all the activities we do with our patients. All professional groups report according to the same framework. The result is a very clean and consistent documentation and an excellent doctor’s report. Transfer of learning is particularly important to us – which brings us to the topic of evaluation. Starting with the question: What can the patient achieve in therapy? For example, a transfer or change of position with forty percent initiative – let’s see what actually sticks in everyday life. This is the biggest challenge. Often we see that patients have some ability in therapy, but for various reasons that ability isn’t always there in everyday life. This is what needs to be worked on. In addition, we also use standardised assessments in the individual treatment fields in order to objectify relevant parameters both clinically and therapeutically. We always have students in our practice who are still studying. That’s great, because they always check what we are doing with a scientific expectation that everything is up to date. We’re never bored (laughs).
Interviewer: I can very well believe it. I wish you continued success and thank you very much for the interview, Mr Erler.
Interviewer: What exactly are the effects of combining the therapies in this way?
Torsten Erler: We experience a significant increase in patient vigilance. Through verticalisation, we achieve conditions for an ideal alignment of the body with respect to gravity, where the head is first of all positioned and swallowing is physiologically possible. This is also possible when lying down or sitting, but it is often much better when standing. Sometimes we even do gait training, which we interrupt in order to include short swallowing sequences or to do oral stimulation. The device support is simply great. It allows us to work very effectively and efficiently, to make corrections in a few easy steps and create optimal conditions. This is very fortunate and would not be possible without the use of technology.
Interviewer: How do you ensure that the treatments are actually goal-oriented and effective?
Torsten Erler: We have set up our own ICF-based documentation for this purpose. This defines participation and includes all the activities we do with our patients. All professional groups report according to the same framework. The result is a very clean and consistent documentation and an excellent doctor’s report. Transfer of learning is particularly important to us – which brings us to the topic of evaluation. Starting with the question: What can the patient achieve in therapy? For example, a transfer or change of position with forty percent initiative – let’s see what actually sticks in everyday life. This is the biggest challenge. Often we see that patients have some ability in therapy, but for various reasons that ability isn’t always there in everyday life. This is what needs to be worked on. In addition, we also use standardised assessments in the individual treatment fields in order to objectify relevant parameters both clinically and therapeutically. We always have students in our practice who are still studying. That’s great, because they always check what we are doing with a scientific expectation that everything is up to date. We’re never bored (laughs).
Interviewer: I can very well believe it. I wish you continued success and thank you very much for the interview, Mr Erler.
The idea is to get patients standing and walking to activate the torso and head posture reactions in order to improve swallowing quality.
2023-3
Audience
Knowledge
Outpatient Rehabilitation
Section
Therapy & Practice
THERAPY Magazine
Volume-Issue
References:
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.