
THERAPY-Magazin
Expert reporton postural control
Explore how alignment, orientation, and sensory integration shape postural control. Learn how updated body schemas and sensor feedback improve stability and mobility in therapy.

Marc Michielsen
Advanced Bobath Instructor
We all live with gravity – usually without thinking that we might fall. This is prevented by an integrated posture control mechanism. The first part of our expert report deals with two of four concepts
of postural control: Alignment and orientation.
of postural control: Alignment and orientation.
Postural control is defined as “the ability to control the body position in space for stability and orientation” [13]. We often take this for granted, because we usually do not have to think about it at all. We only realise it when we see the risk of losing it.
The processing mechanism of postural control must solve two fundamental problems: Orientation and balance of the supporting apparatus. We must continuously control the movement of our body via a more or less stable supporting surface. The task of postural balance involves the coordination of movement strategies in order to stabilise the centre of body mass during self-induced and externally triggered disturbances of balance.
Postural orientation involves the active alignment of the back and head in relation to gravity, support surfaces on which the person stands, the visual environment and internal references. The visual environment is involved to maintain balance and the body is stimulated to perform tasks more efficiently through memories. If the postural orientation is missing, the body would move like a puppet with too much leeway. Therefore the postural orientation controls the movement using precise sensor information. For it to be successful, senses that are distributed over the entire body are integrated.
After a stroke or similar illness, the underlying neurophysiological system that controls posture is impaired. Knowledge of these systems helps therapists to improve their patients’ balance and mobility, thus preventing falls and laying the foundations for certain efficient activities.
The systems approach of Bernstein (1967) was expanded by Shumway-Cook and Woollacott (2007), who emphasised that human motor behaviour is based on continuous interaction between the individual, the task at hand, and the environment. Postural control is located at the intersection of these three domains (Fig. 1).
The processing mechanism of postural control must solve two fundamental problems: Orientation and balance of the supporting apparatus. We must continuously control the movement of our body via a more or less stable supporting surface. The task of postural balance involves the coordination of movement strategies in order to stabilise the centre of body mass during self-induced and externally triggered disturbances of balance.
Postural orientation involves the active alignment of the back and head in relation to gravity, support surfaces on which the person stands, the visual environment and internal references. The visual environment is involved to maintain balance and the body is stimulated to perform tasks more efficiently through memories. If the postural orientation is missing, the body would move like a puppet with too much leeway. Therefore the postural orientation controls the movement using precise sensor information. For it to be successful, senses that are distributed over the entire body are integrated.
After a stroke or similar illness, the underlying neurophysiological system that controls posture is impaired. Knowledge of these systems helps therapists to improve their patients’ balance and mobility, thus preventing falls and laying the foundations for certain efficient activities.
The systems approach of Bernstein (1967) was expanded by Shumway-Cook and Woollacott (2007), who emphasised that human motor behaviour is based on continuous interaction between the individual, the task at hand, and the environment. Postural control is located at the intersection of these three domains (Fig. 1).
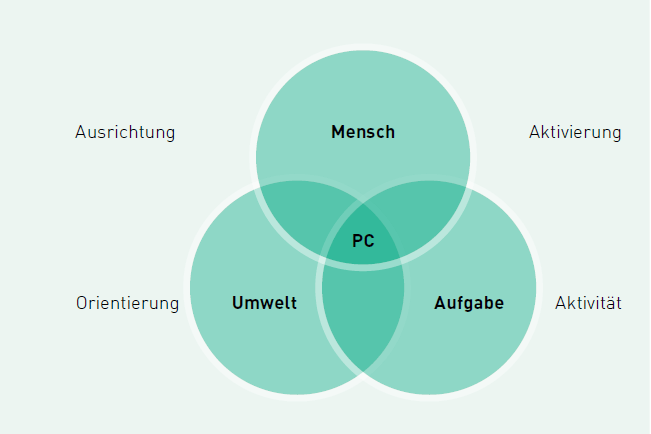
Fig. 1: In order to structure the assessment of postural control and movement, the concepts of alignment, orientation, activation and activity can be helpful.
At a glance Summarised
1.Postural control is concerned with orientation and balance of the supporting apparatus. The movement of the body must be continuously controlled by precise sensor information.
2.To structure the assessment of postural control and movement, the concepts of alignment, orientation, activation and functional activity can be helpful. Knowledge of these systems helps therapists to improve the balance and mobility of their patients.
3.The sensory orientation should be trained in order to be able to perform more precise movements. By analysing the postural alignment, the therapist can assess how a patient will move after therapy.
1.Postural control is concerned with orientation and balance of the supporting apparatus. The movement of the body must be continuously controlled by precise sensor information.
2.To structure the assessment of postural control and movement, the concepts of alignment, orientation, activation and functional activity can be helpful. Knowledge of these systems helps therapists to improve the balance and mobility of their patients.
3.The sensory orientation should be trained in order to be able to perform more precise movements. By analysing the postural alignment, the therapist can assess how a patient will move after therapy.
In order to structure the assessment of postural control and movement, it is helpful to look at the alignment of individual body parts, sensory orientation, postural activation and functional activity sequentially. We use these concepts to provide guidance for the assessment and treatment of patients with acquired brain damage.
Alignment
The analysis of postural orientation is an important element in the clinical evaluation of stroke patients. The alignment of body parts contains information about symmetry, verticality and willingness to move. In this way, the therapist can measure how the patient’s posture counteracts gravity, how they have moved before and how they will move. These hypotheses can only be made if the proprioceptive interaction with the environment and within the task is taken into account.
The analysis of postural orientation is an important element in the clinical evaluation of stroke patients. The alignment of body parts contains information about symmetry, verticality and willingness to move. In this way, the therapist can measure how the patient’s posture counteracts gravity, how they have moved before and how they will move. These hypotheses can only be made if the proprioceptive interaction with the environment and within the task is taken into account.
The importance of appropriate alignment is evident in the biomechanical properties, neuro-physiological organisation and cardiorespiratory endurance. The postural muscles should be able to work under low energy input to maintain postural control over a longer period of time and adapt to changing support surfaces. Through the appropriate alignment of the body parts, the postural musculature is biomechanically moved into the right area to work with minimal effort.
From a neurophysiological point of view, it is known that motor neurons do not “know” muscles, but instead recognise the movement pattern. Due to the nature of this neuronal organisation, relearning movement patterns is a more important goal than relearning individual muscle contractions. Cortical neurons change the initial value of the fire rate while waiting for a certain movement to occur. Creating a postural set (see Box 1), i.e. aligning body parts in a certain posture, thus increases the probability of neural fire.
Cardiovascular or cardiorespiratory endurance refers to the ability of the body to perform endurance dynamic exercises involving large muscles at moderate intensity. In stroke patients, maintaining an active posture over a longer period of time is a cardiovascular challenge. Patients in a stroke rehabilitation clinic spend 74% of their “active” day sitting or lying down [14]. They spend long periods of time in unsuitable positions [3]. A certain level of fitness is required to participate in the basic activities of everyday life. People who suffer from a disability after a stroke have to spend more energy on many physical activities [7]. During the acute stage of a stroke, postural activities are real challenges. Since the energy required for this is limited, it leads to misalignment and impairment of postural preparation. This in turn leads to poor postural control and restriction of functional activities.
From a neurophysiological point of view, it is known that motor neurons do not “know” muscles, but instead recognise the movement pattern. Due to the nature of this neuronal organisation, relearning movement patterns is a more important goal than relearning individual muscle contractions. Cortical neurons change the initial value of the fire rate while waiting for a certain movement to occur. Creating a postural set (see Box 1), i.e. aligning body parts in a certain posture, thus increases the probability of neural fire.
Cardiovascular or cardiorespiratory endurance refers to the ability of the body to perform endurance dynamic exercises involving large muscles at moderate intensity. In stroke patients, maintaining an active posture over a longer period of time is a cardiovascular challenge. Patients in a stroke rehabilitation clinic spend 74% of their “active” day sitting or lying down [14]. They spend long periods of time in unsuitable positions [3]. A certain level of fitness is required to participate in the basic activities of everyday life. People who suffer from a disability after a stroke have to spend more energy on many physical activities [7]. During the acute stage of a stroke, postural activities are real challenges. Since the energy required for this is limited, it leads to misalignment and impairment of postural preparation. This in turn leads to poor postural control and restriction of functional activities.
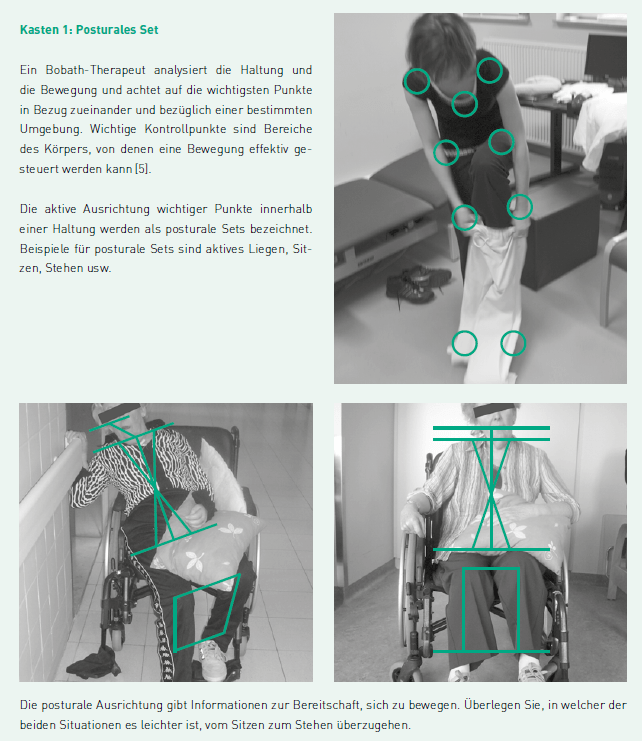
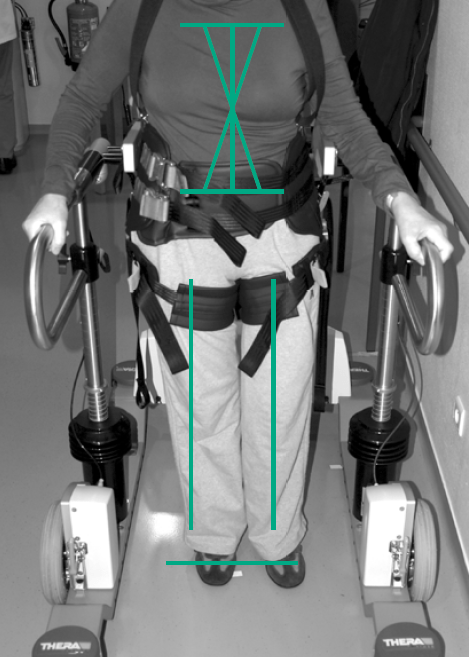
Abb. 2: THERA-Trainer e-go und Ausrichtung
Sensory orientation
In order to understand postural control as an ability, it is important to examine the task and its requirements on a moving body. The body is brought into a vertical position against gravity and correctly aligned with the aid of the support surface and according to the task. For reasons of efficiency, the brain uses a network of various sensory impressions.
In order to understand postural control as an ability, it is important to examine the task and its requirements on a moving body. The body is brought into a vertical position against gravity and correctly aligned with the aid of the support surface and according to the task. For reasons of efficiency, the brain uses a network of various sensory impressions.
Body schema
The body schema is composed of various sensory information and is updated accordingly. In therapy, an important goal is to update the patient’s internal reference system by providing precise, goal-oriented input. An updated body schema improves the efficiency of movement and increases the patient’s ability to interact with their environment and carefully select specific tasks.
In the more recent literature, the body schema is described as an internal model, which is considered a general neural process. It links information from sensory sources and combines incoming and outgoing information. [11] Thus it has the characteristics of a processor. The advantage of an internal model is that it can predict the future, so to speak. The brain can use the body schema to make calculations to develop plans for the future. In doing so, it is dependent on information that it receives continuously. An updated body schema improves the efficiency of movement and increases the patient’s ability to perform a task in a stimulus-enhanced environment. The loss of sensory information, for example in stroke patients, prevents the continuous updating of the body schema and leads to an interruption of postural control.
The body schema is composed of various sensory information and is updated accordingly. In therapy, an important goal is to update the patient’s internal reference system by providing precise, goal-oriented input. An updated body schema improves the efficiency of movement and increases the patient’s ability to interact with their environment and carefully select specific tasks.
In the more recent literature, the body schema is described as an internal model, which is considered a general neural process. It links information from sensory sources and combines incoming and outgoing information. [11] Thus it has the characteristics of a processor. The advantage of an internal model is that it can predict the future, so to speak. The brain can use the body schema to make calculations to develop plans for the future. In doing so, it is dependent on information that it receives continuously. An updated body schema improves the efficiency of movement and increases the patient’s ability to perform a task in a stimulus-enhanced environment. The loss of sensory information, for example in stroke patients, prevents the continuous updating of the body schema and leads to an interruption of postural control.
Sensory processes
Each sensor generates input (receptor activity) about position and movement of the body. This multisensory input is processed by the brain and thus becomes information. The perception process informs the brain about the position and activity of the body relative to the environmental conditions. Based on previous experience and the purpose of the intended movement, the brain chooses efficient strategies for postural control.
Sensory receptors and systems that are considered in conne
Each sensor generates input (receptor activity) about position and movement of the body. This multisensory input is processed by the brain and thus becomes information. The perception process informs the brain about the position and activity of the body relative to the environmental conditions. Based on previous experience and the purpose of the intended movement, the brain chooses efficient strategies for postural control.
Sensory receptors and systems that are considered in conne
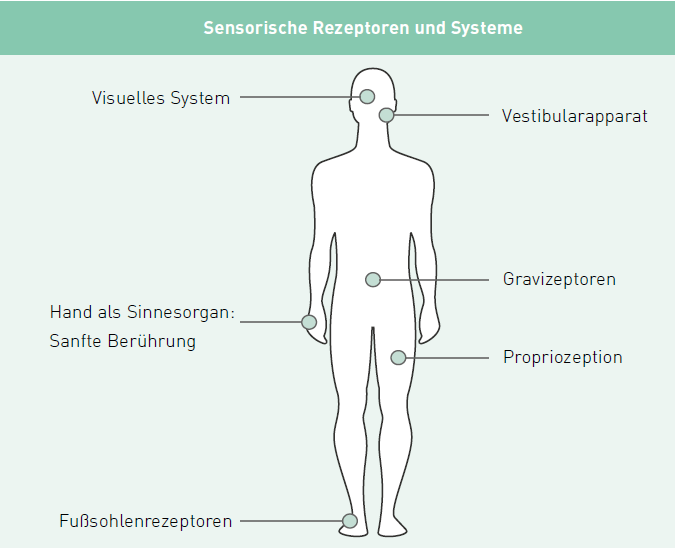
Fig. 3: Sensory receptors and systems associated with postural control
Visual system
In our everyday life we are surrounded by numerous horizontal and vertical references such as windows, tables or chairs. The subjective vertical view (SVV) gives an indication of verticality. Healthy people can perceive vertical lines very precisely thanks to their visual abilities.
Another important contribution to the visual input for postural control is the optical flow. This refers to the perceived movement of the field of vision, which results from the movement of a person in their environment. On the one hand, the optical flow contains information about postural control by perceiving the faint movements resulting from body sway. On the other hand, it contains information about the organisation of the environment and indicates that closer objects move faster than those further away. By integrating different sensory systems, the body is informed whether it is moving relative to the environment or whether the environment is moving relative to the body.
In our everyday life we are surrounded by numerous horizontal and vertical references such as windows, tables or chairs. The subjective vertical view (SVV) gives an indication of verticality. Healthy people can perceive vertical lines very precisely thanks to their visual abilities.
Another important contribution to the visual input for postural control is the optical flow. This refers to the perceived movement of the field of vision, which results from the movement of a person in their environment. On the one hand, the optical flow contains information about postural control by perceiving the faint movements resulting from body sway. On the other hand, it contains information about the organisation of the environment and indicates that closer objects move faster than those further away. By integrating different sensory systems, the body is informed whether it is moving relative to the environment or whether the environment is moving relative to the body.
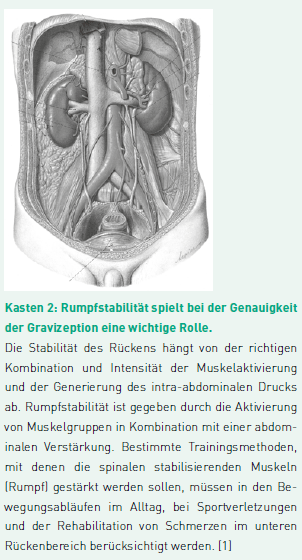
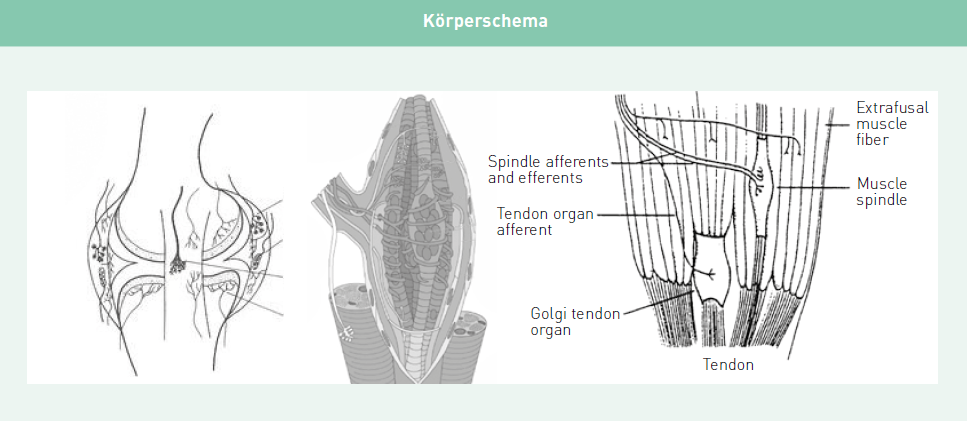
Fig. 4: Information from joint receptors, muscle spindles and the Golgi tendon organs together form the body schema
Vestibular apparatus
Although there are no overtly conscious sensations from the vestibular organs, their signals contribute to an astonishingly large proportion of brain functions. [2] In a far more conscious way, the vestibular apparatus passes on information about egocentric and exocentric movements.
The main task of the saccule and utricle is to keep the head in a vertical orientation with respect to gravity. When the head and body tilt, the vestibular apparatus automatically steers against it with the correct postural adjustment. The vestibular information is strongly combined with visual input, eye muscle and neck proprioception.
Although there are no overtly conscious sensations from the vestibular organs, their signals contribute to an astonishingly large proportion of brain functions. [2] In a far more conscious way, the vestibular apparatus passes on information about egocentric and exocentric movements.
The main task of the saccule and utricle is to keep the head in a vertical orientation with respect to gravity. When the head and body tilt, the vestibular apparatus automatically steers against it with the correct postural adjustment. The vestibular information is strongly combined with visual input, eye muscle and neck proprioception.
Graviceptors
Somatic graviceptors are mediated by two clearly defined inputs. [10] The exact function of these inputs has yet to be clarified. Mittelstaedt describes that bilateral nephrectomy influences the perception of gravity in paraplegic patients. This means that receptors in the kidney can influence the perception of verticality. One hypothesis is that the second input comes from receptors in the large abdominal vessels. Gravity information can result from the inertia of the blood mass in these vessels.
A strong, efficient back can increase the efficiency of the input to the graviceptors. In stroke patients, a lack of trunk stability can lead to a decrease in the efferent dynamics of the medial descending nerve tracts and influence the accuracy of the graviceptors, resulting in a reduced perception of gravity.
Somatic graviceptors are mediated by two clearly defined inputs. [10] The exact function of these inputs has yet to be clarified. Mittelstaedt describes that bilateral nephrectomy influences the perception of gravity in paraplegic patients. This means that receptors in the kidney can influence the perception of verticality. One hypothesis is that the second input comes from receptors in the large abdominal vessels. Gravity information can result from the inertia of the blood mass in these vessels.
A strong, efficient back can increase the efficiency of the input to the graviceptors. In stroke patients, a lack of trunk stability can lead to a decrease in the efferent dynamics of the medial descending nerve tracts and influence the accuracy of the graviceptors, resulting in a reduced perception of gravity.
Gentle touch as a supporting aid
Lightly touching a firm surface with the hand provides orientation or reference that enhances control of upright posture by increasing axial tone [6, 12]. Kouzaki (2008) points out that the reduced postural swaying when standing still while lightly touching a firm surface is due to the tactile feedback of the fingers and not to mechanical support. These findings support the importance of activating the hand as a sensory organ. The concept of light touch cannot be stressed enough. If a patient can support their weight with their upper limbs, postural reactions include the extensor muscles of the arm and not those of the legs. [9] In other words, in the latter case the arm is used as a leg, so to speak. If, however, the hand is not part of contact-based therapy, patients miss an opportunity to orient themselves in relation to their surroundings.
A “wake-up call” to activate the receptors in the hand and a well-chosen object from the surroundings can improve sensory perception.
Lightly touching a firm surface with the hand provides orientation or reference that enhances control of upright posture by increasing axial tone [6, 12]. Kouzaki (2008) points out that the reduced postural swaying when standing still while lightly touching a firm surface is due to the tactile feedback of the fingers and not to mechanical support. These findings support the importance of activating the hand as a sensory organ. The concept of light touch cannot be stressed enough. If a patient can support their weight with their upper limbs, postural reactions include the extensor muscles of the arm and not those of the legs. [9] In other words, in the latter case the arm is used as a leg, so to speak. If, however, the hand is not part of contact-based therapy, patients miss an opportunity to orient themselves in relation to their surroundings.
A “wake-up call” to activate the receptors in the hand and a well-chosen object from the surroundings can improve sensory perception.
Proprioception
Information from connected receptors, muscle spindles and the Golgi tendon organs are of utmost importance for constructing and updating the body schema.
Most of the joint receptors fire at the end of the joint movement. Muscle spindles provide proprioception information on the length and rate of muscle length change. This information is transmitted to the spinal cord, the cerebellum and the cortex. They provide information on muscle tension. Golgi tendon organs have a low stimulation threshold (and therefore high responsiveness) to trigger an active muscle contraction and a high threshold (or no response) to stretch the muscle.
An important condition for these receptors to work properly is the contraction of the muscle. Paresis or paralysis of a muscle has a negative effect on the function of the Golgi tendon organ, whereby muscle spindles prevent or slow down the updating of the body schema. In stroke patients, it is important to activate the muscles to regain the efficiency of the proprioceptive input and thus update the body schema. The concept is based on the method “Use it or lose it”.
Information from connected receptors, muscle spindles and the Golgi tendon organs are of utmost importance for constructing and updating the body schema.
Most of the joint receptors fire at the end of the joint movement. Muscle spindles provide proprioception information on the length and rate of muscle length change. This information is transmitted to the spinal cord, the cerebellum and the cortex. They provide information on muscle tension. Golgi tendon organs have a low stimulation threshold (and therefore high responsiveness) to trigger an active muscle contraction and a high threshold (or no response) to stretch the muscle.
An important condition for these receptors to work properly is the contraction of the muscle. Paresis or paralysis of a muscle has a negative effect on the function of the Golgi tendon organ, whereby muscle spindles prevent or slow down the updating of the body schema. In stroke patients, it is important to activate the muscles to regain the efficiency of the proprioceptive input and thus update the body schema. The concept is based on the method “Use it or lose it”.
Receptors on the sole of the foot
The main receptors responsible for stress are the Golgi tendon organs and the cutaneous receptors on the sole of the foot. [4] There are over 104 different cutaneous mechanoreceptors on the smooth skin of the sole of the foot. These mechanoreceptors play an important role in balance and movement control. The tactile afferences of the feet provide the CNS with information about the body position with respect to the vertical axis, which determines the posture in space and the ground on which the feet stand. Tactile sensitivity can be understood as an exteroceptive modality. With regard to postural control, tactile inputs from the sole of the foot have a proprioceptive function that contributes directly to the body’s representation. Kavounnoudias (2001) concludes that the regulation of small amplitude fluctuations of the body is mainly due to tactile inputs from the sole of the foot.
The main receptors responsible for stress are the Golgi tendon organs and the cutaneous receptors on the sole of the foot. [4] There are over 104 different cutaneous mechanoreceptors on the smooth skin of the sole of the foot. These mechanoreceptors play an important role in balance and movement control. The tactile afferences of the feet provide the CNS with information about the body position with respect to the vertical axis, which determines the posture in space and the ground on which the feet stand. Tactile sensitivity can be understood as an exteroceptive modality. With regard to postural control, tactile inputs from the sole of the foot have a proprioceptive function that contributes directly to the body’s representation. Kavounnoudias (2001) concludes that the regulation of small amplitude fluctuations of the body is mainly due to tactile inputs from the sole of the foot.
Ambulante Rehabilitation
balo
Fachkreise
Produkte
Standing & Balancing
Therapy & Practice
THERAPY 2020-I
THERAPY Magazine

Marc Michielsen
Advanced Bobath Instructor
Marc Michielsen studied Physiotherapy at the University of Leuven, Belgium, and is also an Advanced Bobath Instructor. His area of expertise is neurological rehabilitation, particularly following a stroke. After holding several positions as a senior physiotherapist at various hospitals, he has been the Head of Emergency Services at the Rehabilitation Center of Jessa Hospital since 2008. Michielsen has published several articles, abstracts, and other scientific papers in prominent journals.
References:
- Abenhaim L et al. (2000). The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. In: Spine 25(4Suppl): S. 1-33.
- Angelaki DE, Cullen KE (2008). Vestibular system: the many facets of a multimodal sense. In Annual Review of Neuroscience, S. 125-150.
- Dowswell G et al. (2000). Investigating recovery from stroke: a qualitative study. In: Journal of Clinical Nursing, S. 507-515.
- Duysens J et al. (2000). Load-regulating mechanisms in gait and posture: comparative aspects. In: Physiological Reviews, S. 83-133.
- Edwards M (1996). New approaches to children and development: Introduction and overview. In: Journal of International Development, 8 (6), S. 849-858.
- Franzén E et al. (2011). Haptic touch reduces sway by increasing axial tone. In: Neuroscience, Vol. 174, S. 216-223.
- Ivey FM (2006). Exercise rehabilitation after stroke. In: Neurotherapeutics, October 2006, Volume 3, Issue 4, S. 439-450.
- Jeka J (1998). Position and velocity coupling of postural sway to somatosensory drive. In: Journal of Neurophysiology, Vol. 47, No. 4, S. 1661-1674.
- Massion J, Woollacott MH (1996). Posture and equilibrium. In: Bornstein AM, Brandt T, Woollacott MH, editors. In: Clinical Disorders of Balance, Posture and Gait. USA: Oxford University Press, Inc, New York. S. 10-18.
- Mittelstaedt ML, Mittelstaedt H (1996). The influence of oto- liths and somatic graviceptors on angular velocity estimation. In: Journal of Vestibular Research, Res 6, S. 355-366.
- Pérennou DA et al. (2000). The polymodal sensory cortex is crucial for controlling lateral postural stability: evidence from stroke patients. In: Brain Research Bulletin, 53(3), S. 359-365.
- Rabin E (2008). Influences of Arm Proprioception and Degrees of Freedom on Postural Control With Light Touch Feedback. In: Journal of Neurophysiology, 99(2), S. 595-604.
- Shumway-Cook A et al. (2007). Motor Control: Translation Research Into Clinical Practice, Lippincott Williams & Wilkins, 2007.
- Sjöholm A et al. (2014). Sedentary behaviour and physical activity of people with stroke in rehabilitation hospitals. In: Stroke Research and Treatment, Vol. 14, Article ID 597897.
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.