THERAPY Magazin
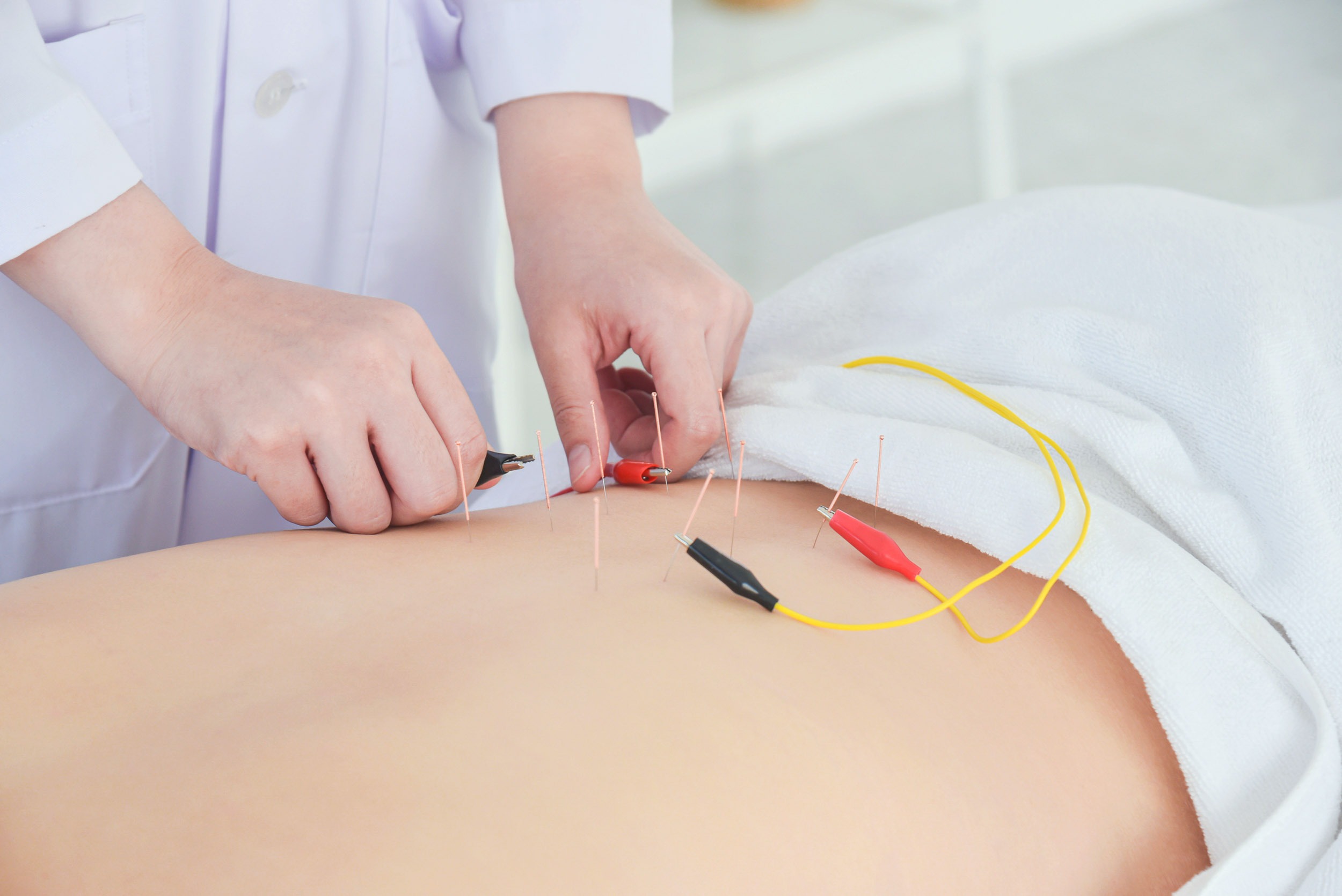
Cycling combined with electrical stimulation at acupuncture points
A Vietnamese study suggests that cycling combined with electrical stimulation at acupuncture points may improve post-stroke recovery. Early results are encouraging – more research is needed.

Jakob Tiebel
Health Business Consultant
An effectiveness analysis of the application of cyclical movement training in combination with electrical stimulation at acupuncture points compared to the exclusive application of electroacupuncture in post-stroke hemiplegia.
Electroacupuncture combined with cyclical movement training could improve the rehabilitation of stroke patients, but the evidence is not yet conclusive. While initial studies show positive effects on muscle power and motor functions, the effectiveness of the combination therapy remains controversial. A recent study from Vietnam suggests that the integration of these methods could bring benefits, but further research is needed to confirm the actual effectiveness and long-term effects.
Electroacupuncture, i.e. the electrical stimulation of acupuncture points, can be used in the treatment of stroke patients to improve motor performance after a stroke. Although the efficacy is not fully understood, there is evidence from animal models and clinical studies that show positive effects.
A systematic review from 2018, which included 19 studies with a total of 1434 participants, reported a superior effectiveness of electroacupuncture when used in combination with conventional therapy with regard to the restoration of motor functions after a stroke [1].
Numerous studies also emphasise that recovery after a stroke can be improved by cyclical movement training, as it has positive effects on motor performance and neuronal networking (see p. 18 “Cycling improves walking performance after stroke” in this issue) [2,3].
In order to achieve the most effective recovery of motor functions after a stroke, electrical stimulation can be applied to acupuncture points in conjunction with rehabilitation measures. Such combination therapies have already been shown to be effective in improving muscular sensitivity, function and movement coordination [4,5,6].
Electroacupuncture, i.e. the electrical stimulation of acupuncture points, can be used in the treatment of stroke patients to improve motor performance after a stroke. Although the efficacy is not fully understood, there is evidence from animal models and clinical studies that show positive effects.
A systematic review from 2018, which included 19 studies with a total of 1434 participants, reported a superior effectiveness of electroacupuncture when used in combination with conventional therapy with regard to the restoration of motor functions after a stroke [1].
Numerous studies also emphasise that recovery after a stroke can be improved by cyclical movement training, as it has positive effects on motor performance and neuronal networking (see p. 18 “Cycling improves walking performance after stroke” in this issue) [2,3].
In order to achieve the most effective recovery of motor functions after a stroke, electrical stimulation can be applied to acupuncture points in conjunction with rehabilitation measures. Such combination therapies have already been shown to be effective in improving muscular sensitivity, function and movement coordination [4,5,6].
The authors conclude that the combination of electrical stimulation at acupuncture points with cyclical movement training has a positive influence on the motor recovery of stroke patients.

In this context, a research group from the Department of Senior Specialist National Hospital for Traditional Medicine and Acupuncture in Vietnam recently investigated the effects of cyclical movement training in combination with electroacupuncture compared with the exclusive use of electroacupuncture in patients with hemiplegia following a stroke. The researchers conducted a randomised control study for this purpose.
Methods
The outcome-assessor-blinded randomised controlled study was designed and conducted in the clinics of the Vietnamese institute. A total of 120 patients with post-stroke hemiplegia were randomly divided into two groups: electrical stimulation of acupuncture points in combination with cyclical movement training (IG) and electrical stimulation of acupuncture points alone (CG). Patients were assessed before and after treatment using muscle contraction, modified Rankin score, Barthel index, Orgogozo score and electromyography. Non-parametric statistical evaluation methods were used to analyse the differences between the groups.
The outcome-assessor-blinded randomised controlled study was designed and conducted in the clinics of the Vietnamese institute. A total of 120 patients with post-stroke hemiplegia were randomly divided into two groups: electrical stimulation of acupuncture points in combination with cyclical movement training (IG) and electrical stimulation of acupuncture points alone (CG). Patients were assessed before and after treatment using muscle contraction, modified Rankin score, Barthel index, Orgogozo score and electromyography. Non-parametric statistical evaluation methods were used to analyse the differences between the groups.
Intervention
In addition to the usual rehabilitation programme, the participants in the IG received 30 minutes of cyclical leg movement training every day, five days a week. The training protocol comprised two training modes, which were carried out and recorded by a qualified physiotherapist.
1) Passive training: for patients with muscle power 0, 1 or 2, at a speed of 20 revolutions per minute (rpm).
2) Active training with/without resistance: for patients with muscle power 3 – 5, at a speed of 60 rpm, focussing on the best performance of the load symmetry of the lower extremities.
In addition to the usual rehabilitation programme, the participants in the IG received 30 minutes of cyclical leg movement training every day, five days a week. The training protocol comprised two training modes, which were carried out and recorded by a qualified physiotherapist.
1) Passive training: for patients with muscle power 0, 1 or 2, at a speed of 20 revolutions per minute (rpm).
2) Active training with/without resistance: for patients with muscle power 3 – 5, at a speed of 60 rpm, focussing on the best performance of the load symmetry of the lower extremities.
Although the study shows positive effects, the evidence base remains weak, which is why further studies are needed to validate the long-term effects and the specific effect of the combination therapy.

Results
The results showed a statistically significant improvement in motor function in both groups. Patients in the IG achieved better results com-pared to those in the CG. These included improved muscle contraction (increased frequency and amplitude of electromyography and improved strength values), improved recovery (measured by the Orgogozo score), increased independence (measured by the Barthel index) and reduced disability (measured by the modified Rankin score).
The results showed a statistically significant improvement in motor function in both groups. Patients in the IG achieved better results com-pared to those in the CG. These included improved muscle contraction (increased frequency and amplitude of electromyography and improved strength values), improved recovery (measured by the Orgogozo score), increased independence (measured by the Barthel index) and reduced disability (measured by the modified Rankin score).
Conclusions
The authors conclude that the combination of electrostimulation at acupuncture points with cyclical movement training has a positive influence on the recovery of stroke patients. The results indicate that the integration of cyclical movement training in the treatment of patients with post-stroke hemiplegia in combination with electroacupuncture is a promising method for improving motor function.
The authors conclude that the combination of electrostimulation at acupuncture points with cyclical movement training has a positive influence on the recovery of stroke patients. The results indicate that the integration of cyclical movement training in the treatment of patients with post-stroke hemiplegia in combination with electroacupuncture is a promising method for improving motor function.
Commentary on the study
In the present study, a statistically significant improvement in certain motor functions was observed in patients with hemiplegia after an ischaemic stroke. Positive effects were seen both in the group that received electroacupuncture alone and in the group that additionally performed 30 minutes of cyclical movement training with moderate exertion.
The effects were stronger in the patients in the intervention group, which is consistent with previous studies. However, the evidence base remains weak. The present study has some limitations. These included an insufficient sample size, a relatively limited intervention duration, possible distortions due to the open study design and weaknesses in the statistical analysis. The authors also recognise this in their publication. Further studies are therefore needed to validate the efficacy and long-term effects of the therapy. In particular, the extent to which the combination of cyclical movement training and electrostimulation at acupuncture points increases the effects must be critically examined. This is because it cannot be ruled out that the effects of the individual therapies merely add up. In the past, both electroacupuncture and cyclical movement training have independently shown positive effects on the endpoints studied.
In the present study, a statistically significant improvement in certain motor functions was observed in patients with hemiplegia after an ischaemic stroke. Positive effects were seen both in the group that received electroacupuncture alone and in the group that additionally performed 30 minutes of cyclical movement training with moderate exertion.
The effects were stronger in the patients in the intervention group, which is consistent with previous studies. However, the evidence base remains weak. The present study has some limitations. These included an insufficient sample size, a relatively limited intervention duration, possible distortions due to the open study design and weaknesses in the statistical analysis. The authors also recognise this in their publication. Further studies are therefore needed to validate the efficacy and long-term effects of the therapy. In particular, the extent to which the combination of cyclical movement training and electrostimulation at acupuncture points increases the effects must be critically examined. This is because it cannot be ruled out that the effects of the individual therapies merely add up. In the past, both electroacupuncture and cyclical movement training have independently shown positive effects on the endpoints studied.
Cycling
Fachkreise
Produkte
Stationäre Rehabilitation
Technology & Development
THERAPY 2024-II
THERAPY Magazine

Jakob Tiebel
Health Business Consultant
Jakob Tiebel is OT and studied applied psychology with a focus on health economics. He has clinical expertise from his previous therapeutic work in neurorehabilitation. He conducts research and publishes on the theory-practice transfer in neurorehabilitation and is the owner of an agency for digital health marketing.
References:
- Electroacupuncture as an adjunctive therapy for motor dysfunction in acute stroke survivors: a systematic review and Meta-analyses. BMJ Open 2018; 8: e017153.
- Klarner T, Barss TS, Sun Y, Kaupp C, Zehr EP. Preservation of common rhythmic locomotor control despite weakened supraspinal regulation after stroke. Front Integr Neurosci 2014; 8: 95.
- Tanuma A, Fujiwara T, Yamaguchi T, et al. After-effects of pedaling exercise on spinal excitability and spinal reciprocal inhibition in patients with chronic stroke. Int J Neurosci 2017; 127: 73-9.
- Wei NN, Pan JX, Chen YP, Chen Y. Effects of balance acupuncture combined with motor relearning for lower limb motor function of stroke patients with hemiplegia. Zhen Ci Yan Jiu 2018; 43:730-2.
- Chen L, Fang J, Ma R, et al. Additional effects of acupuncture on early comprehensive rehabilitation in patients with mild to moderate acute ischemic stroke: a multicenter randomized controlled trial. BMC Complement Altern Med 2016; 16: 226.
- Zhao DG, Mu JP. Clinical study on scalp acupuncture combined with sports therapy for rehabilitation of poststroke hemiplegia. Zhong Guo Zhen Jiu 2005; 25: 19-20.
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.
You need to load content from reCAPTCHA to submit the form. Please note that doing so will share data with third-party providers.
More InformationYou are currently viewing a placeholder content from Turnstile. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More Information