
Discover how neurological balance disorders can be treated effectively. This article outlines motor, sensory, and cognitive deficits after stroke—and presents evidence-based therapy using an interaction model and structured taxonomy.

All aspects of the individual, including motor skills, sensory perception, and cognition, can be affected by neurological disorders. Accordingly, the disorders set out below (following neurological disease) can be assigned, based on the interaction model.
- lack of anti-gravity muscle activity
- restricted postural synergies (e.g. ankle strategy (upper ankle joint), protective steps)
- In addition, limitations in joint mobility (often due to adaptive phenomena of the musculature, particularly in the upper ankle area) may play a role
- limited surface and depth sensitivity, particularly in the area of the feet
- limited ability for sensory weighting
- a strongly-altered body schema (e.g. in patients who push or who exhibit a neglect)
- limited dual-task capability
- reduced problem-solving ability
- reduced self-efficacy
- Unsteadiness when standing freely
-Increased use of the upper extremities (UE) (holding on, durable medical equipment)
- Restricted upper ankle strategy, increased use of the hip joint strategy
- (Very) restricted stability limits (cone of stability) when standing
- Restricted, slowed lateral weight transfer, particularly to the more affected side (asymmetry)
- Inability to perform single-leg stance
- Slowed change from double-leg to single-leg stance
- Visual fixation (visual acuity dependency)
-Blickfixation (Visusabhängigkeit)
Of course, this depends heavily on the individual (motor, sensory and cognitive) disorder pattern. For some patients, the steady-state situation can itself be difficult. For others, the challenge lies primarily in dynamic-anticipatory and/or reactive tasks. Investigations indicate that unsteadiness and falls can often occur during transfers, when walking (and turning), during the transition from sitting to standing, but also when standing [3, 5, 20, 21].
Environmental factors such as unevenness, unstable and/or sloping surfaces [14] as well as restricted light conditions [12] similarly influence balance behaviour and should therefore be taken into account in therapy.
The different disorder patterns outlined above can be influenced through therapy. There is evidence for the effectiveness of interventions that specifically train particular aspects of motor skills, sensory perception or cognition.
In order to structure the interventions, the interaction model can provide a practical framework (see Issue I/2018).
- postural synergies (upper ankle strategy):
- improved performance [6, 16]
- increased speed [19]
- anticipatory postural control: improved weight transfers when standing [25]
- protective steps: improved, faster performance [15, 18]
Examples of evidence for treatment of the cognitive component:
dual-task capability: improvement [23]
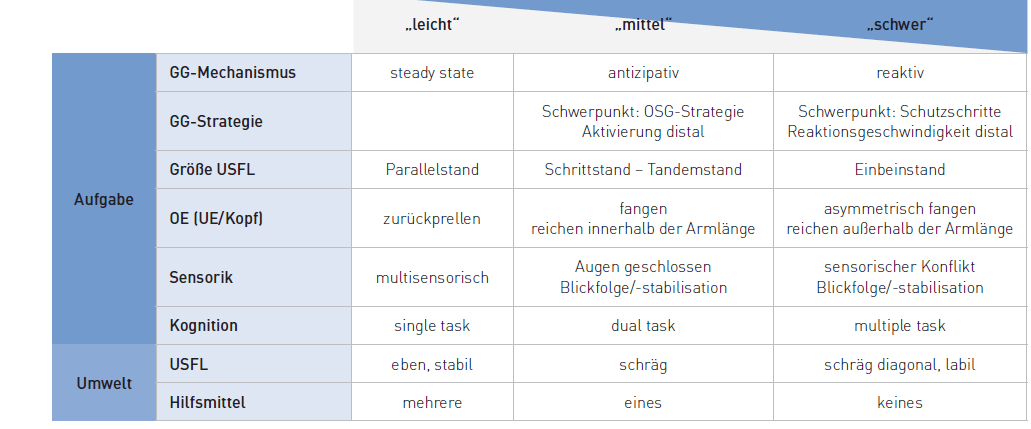
For the systematic and structured design of balance training, the application of what is termed a taxonomy (system) is proposed. This system is based on the interaction model and offers the possibility of being able to offer highly patient-centred and goal-oriented therapy through the targeted application of task and environmental parameters (see Fig. 1). This taxonomy is also the basis of THERA-soft for the THERA-Trainer standing & balancing devices.
The taxonomy is perfectly compatible with the current evidence. Both results from individual studies as well as conclusions from reviews [1, 2, 28, 29] and recommendations from guidelines [8, 9, 17, 26] can easily be integrated into this system.
For example, the KNGF Stroke Guideline (2014) from the Dutch Professional Association of Physiotherapy makes the following recommendation: “Practicing balance during various activities improves balance when sitting and standing and performing basic activities of daily living (ADL).”
The Guideline of the Australian Stroke Foundation (2017) suggests that “task-oriented practising of standing balance should be offered to patients who have difficulty standing. This can include the performance of functional tasks when standing.”
The common basis of both recommendations is the task-oriented approach. This essentially means practising the thing that needs improvement. “The interventions are also designed in such a way that the person practising can develop efficient and effective (task-specific) strategies to solve functional, meaningful and individually-relevant tasks” [13]. Using the taxonomy, task-oriented balance training can be systematically, practically and individually created. Shaping (continuous and systematic adaptation of the task level to the current performance of the person practising), as one of the most important principles of motor learning, can also be designed specifically with it.

- Aman J. E. (2015) The effectiveness of proprioceptive training for improving motor function: a systematic review, Front Hum Neurosci. 8:1075.
- An M. (2011) The effects of exercise-based rehabilitation on balance and gait for stroke patients: a systematic review. J Neurosci Nurs. 43(6):298-307.
- Batchelor F. et al. (2012) Falls after stroke. International Journal of Stroke.
- Bonan I. V. (2004) Reliance on visual information after stroke. Part II: Effectiveness of a balance rehabilitation program with visual cue deprivation after stroke: a randomized controlled trial. Arch Phys Med Rehabil;85:274-8.
- Cheng F.-Y., (2014) Factors Influencing Turning and Its Relationship with Falls in Individuals with Parkinson’s Disease. PLoS ONE 9(4): e93572.
- Davies B. L. (2015) Neurorehabilitation Strategies Focusing on Ankle Control Improve Mobility and Posture in Persons With Multiple Sclerosis. J Neurol Phys Ther. 39(4):225-32.
- de Haart M. (2004) Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil 85:886-95.
- Dohle Ch. (2015) Rehabilitation der Mobilität nach Schlaganfall (ReMoS). S2e-Leitlinie. Neurologie & Rehabilitation 7.
- EBRSR (2016) The Stroke Rehabilitation Clinician’s Handbook. Download am 07.05.2018 unter http://www.ebrsr.com/clinician-handbook.
- Gandolfi M. (2015) Sensory integration balance training in patients with multiple sclerosis: A randomized, controlled trial. Mult Scler. 21(11):1453-62.
- Geurts A. C. (2005) A review of standing balance recovery from stroke. Gait Posture 22(3):267-81.
- Horak F. B. (2006) Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls. Age Ageing. 35 Suppl 2:ii7-ii11.
- Huber M. (2016) „Posturale Kontrolle – Grundlagen.“ Neuroreha (Thieme-Verlag). 8: 158-162.
- Huber M. (2018) Balancepad – wissen wir wie’s wirkt? physiopraxis 2018; 16(5):30-31.
- Jöbges M. (2004) Repetitive training of compensatory steps: a therapeutic approach for postural instability in Parkinson’s disease J Neurol Neurosurg Psychiatry.75:1682-1687.
- Kitatani R. et al. (2016) Ankle muscle coactivation during gait is decreased immediately after anterior weight shift practice in adults after stroke. Gait & Posture 45:35-40.
- KNGF (2014) Clinical Practice Guideline for Physical Therapy in patients with stroke. https://www.fysionet-evidencebased.nl/index.php/kngf-guidelines-in-english.
- Mansfield A. (2011) Training rapid stepping responses in an individual with stroke. Phys Ther. 91:958-969.
- Marigold D. C. (2005) Exercise Leads to Faster Postural Reflexes, Improved Balance and Mobility, and Fewer Falls in Older Persons with Chronic Stroke. JAGS 53:416-423.
- Matsuda P. (2011) Falls in Multiple Sclerosis, PM&R 3;(7) : 624-632.
- Robinovitch S. N. (2013) Video capture of the circumstances of falls in elderly people residing in long term care: an observational study. Lancet 381(9860): 47-54.
- Shumway-Cook A., Woollacott M. J. (2016) Motor Control 5th Edition Lippincott Raven.
- Silsupadol P. et al. (2006) Training of balance under single and dual-task conditions in older adults with balance impairment. PhysTher. 86:269-281.
- Smania N. (2008) Rehabilitation of sensorimotor integration deficits in balance impairment of patients with stroke hemiparesis: a before/after pilot study. Neurol Sci. 29:313-319.
- Sparrow D. (2016) Highly Challenging Balance Program Reduces Fall Rate in Parkinson Disease. J Neurol Phys Ther.40(1):24-30.
- Stroke Foundation (2017) Clinical Guidelines for Stroke Management. Melbourne Australia. https://informme.org.au/Guidelines/Clinical-Guidelines-for-Stroke-Management-2017.
- Tasseel-Ponche S. (2015) Motor strategies of postural control after hemispheric stroke. Neurophysiol Clin. 45(4-5):327-33
- van Duijnhoven H. J. (2016) Effects of Exercise Therapy on Balance Capacity in Chronic Stroke: Systematic Review and Meta-Analysis. Stroke. 47(10):2603-10.
- Veerbeek J. M. (2014) What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis. PLoS ONE 9(2): e87987.
Related contents
Find related exciting contents in our media library.
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.
You need to load content from reCAPTCHA to submit the form. Please note that doing so will share data with third-party providers.
More InformationYou are currently viewing a placeholder content from Turnstile. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More Information