
THERAPY-Magazin
Device-aided balance training for people with stroke
A study shows how device-supported balance training at home improves mobility and stability in stroke patients. Learn more about methods, results, and outcomes.

Anis Hamila
Physiotherapeut
A clinical study on the feasibility and effectiveness of dynamic standing training in the recovery of function for stroke patients living at home.
In many industrial countries, as in Germany, the age structure of the population is changing, with the number of older people increasing. The probability of a stroke increases significantly with age. In 2007, CVD was responsible for around 15% of all hospital stays for people aged 65 and over [8]. Thanks to improved examination and treatment methods in specialist centres, known as stroke units, the mortality rate has continued to fall in recent years [13].
The pattern of recovery following a stroke is very different from patient to patient [2]. One-third of survivors suffer a life-long disability, which in addition to the physical and mental impairments for the person affected also represent a major burden for the health care system [6]. According to Schaechter, 50% to 60% of stroke patients still suffer motor impairments after the end of standard rehabilitation. Around 50% of them show at least one restriction, with the result that partial dependency influences the activities of daily life (ADL) [9].
Given the many different consequences of a stroke, rehabilitation needs to be multidisciplinary in order to minimise the physical and mental impairments over the long term. The primary goals of rehabilitation in the early phase following a stroke are to improve mobility and to minimise the risk of a fall [11]. Regaining lost motor skills is the goal of many measures in the later phase, which represents a major challenge in addition to the age-related deterioration in these skills. Improving mobility and minimising the risk of a fall in the chronic phase (from 6 months following a stroke) are fundamental for the patient’s individual recovery process.
In order to guarantee participation in daily activities following a stroke, it is important to improve, or at least maintain, mobility in older patients. Several studies show that the key to this lies in a good capacity for balance and in a reduced fear of falling [12,3,10]. Today, medical progress permits the use of new technologies and devices, such as e.g. virtual reality. Many studies show that patients in the chronic phase following a stroke can benefit from such approaches [1][7][4][5].
The “Apparative Balance Training mit Apoplex Betroffenen (ABmAB)” [“Device-based Balance Training with apoplexy sufferers (ABmAB)”] project was launched for scientific establishment of new forms of therapy in the treatment of stroke patients in the chronic phase. This project investigates the effect of a new training method, the BALANCE-Trainer system, on the capacity for balance, mobility and fall-related self-efficacy of stroke patients living at home, and its feasibility. The issue of balance, in particular, will be the focus of the investigation. In doing so, the goal for the future is to develop better interventions for older people following a stroke in order to extend the level of knowledge regarding therapeutic measures.
The pattern of recovery following a stroke is very different from patient to patient [2]. One-third of survivors suffer a life-long disability, which in addition to the physical and mental impairments for the person affected also represent a major burden for the health care system [6]. According to Schaechter, 50% to 60% of stroke patients still suffer motor impairments after the end of standard rehabilitation. Around 50% of them show at least one restriction, with the result that partial dependency influences the activities of daily life (ADL) [9].
Given the many different consequences of a stroke, rehabilitation needs to be multidisciplinary in order to minimise the physical and mental impairments over the long term. The primary goals of rehabilitation in the early phase following a stroke are to improve mobility and to minimise the risk of a fall [11]. Regaining lost motor skills is the goal of many measures in the later phase, which represents a major challenge in addition to the age-related deterioration in these skills. Improving mobility and minimising the risk of a fall in the chronic phase (from 6 months following a stroke) are fundamental for the patient’s individual recovery process.
In order to guarantee participation in daily activities following a stroke, it is important to improve, or at least maintain, mobility in older patients. Several studies show that the key to this lies in a good capacity for balance and in a reduced fear of falling [12,3,10]. Today, medical progress permits the use of new technologies and devices, such as e.g. virtual reality. Many studies show that patients in the chronic phase following a stroke can benefit from such approaches [1][7][4][5].
The “Apparative Balance Training mit Apoplex Betroffenen (ABmAB)” [“Device-based Balance Training with apoplexy sufferers (ABmAB)”] project was launched for scientific establishment of new forms of therapy in the treatment of stroke patients in the chronic phase. This project investigates the effect of a new training method, the BALANCE-Trainer system, on the capacity for balance, mobility and fall-related self-efficacy of stroke patients living at home, and its feasibility. The issue of balance, in particular, will be the focus of the investigation. In doing so, the goal for the future is to develop better interventions for older people following a stroke in order to extend the level of knowledge regarding therapeutic measures.
Background and purpose
Even years after a stroke, many older people living at home suffer from reduced mobility and capacity for balance, and also from an increased risk of falls. Movement therapy and various new training methods, including virtual reality, can improve balance and mobility in patients. The goal of this study is to examine the feasibility and the effectiveness of a new, dynamic standing training method for stroke patients living at home in relation to balance, mobility and fall-related self-efficacy.
Methods
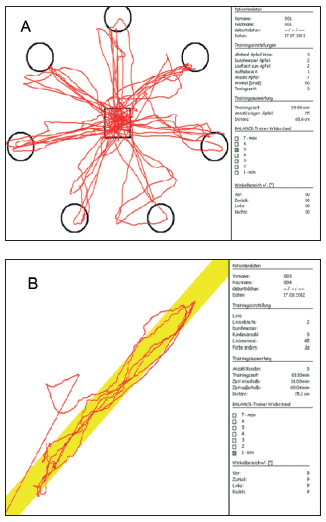
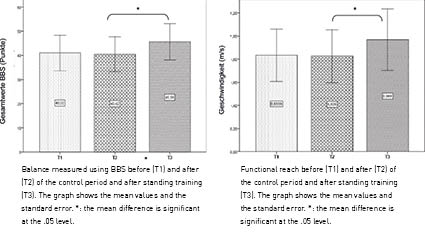
A longitudinal study with a control period based on a cross-over design was carried out. The test subjects (9 men; 3 women, aged 71. 2 ± 5.7 years) trained on 12 training units using a BALANCE-Trainer system. Training took place twice a week over seven weeks. The performance of the test subjects was tested at three points in time (T1, T2 and T3). The period between T1 and T2 represented a control period without training and T3 took place following the end of the intervention period. Tests examined balance (Berg Balance Scale), functional reach (Functional Reach Test), mobility (Timed Up And Go Test), speed of walking over 10 metres, and fall-related self-efficacy (Activities-Specific Balance Confidence Scale).
Results
The low drop-out rate (14.28%) indicates sound feasibility of the training intervention. After training, the test subjects were able to improve significantly (p<.05) in nearly all measured results. On the Berg Balance Scale, the test subjects improved on average from 40.4 ± 12.5 points to 45.6 ± 13 points, on the Functional Reach Test from 13.4 ± 5.1 cm to 17.9 ± 6 cm and on walking speed from 0.82 ± 0.39 m/s to 0.97 ± 0.46m/s. The changes in the Timed Up And Go Test and in fall-related self-efficacy were not statistically significant.

Discussion
The intervention using the BALANCE-Trainer system was suitable for use with stroke patients living at home. The training intervention demonstrated an improvement in balance and mobility. However, these results should be further examined in future studies over a longer period and with more suitable measurement procedures.
Keywords
BALANCE-Trainer, stroke, balance, mobility, fall-related self-efficacy.
2017-1
Audience
balo
coro
Knowledge
Long Term Care
Science
Section
Standing & Balancing
THERAPY Magazine
Training At Home
verto

Anis Hamila
Physiotherapeut
Anis Hamila is a certified physiotherapist who studied at the 'Ecole supérieure des sciences et techniques de la santé de Monastir' in Monastir, Tunisia. In 2010, Anis Hamila began a Master's program with a focus on Movement and Sports Gerontology at the German Sport University in Cologne, where he supported numerous research projects as a research assistant at the institute. As part of his Master's thesis, he focused intensively on the feasibility and effectiveness of dynamic standing training using equipment for stroke patients and conducted a longitudinal study with home-dwelling stroke patients as part of his final thesis
References:
- Cho, K. H., Lee, K. J., & Song, C. H. (2012). Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. The Tohoku journal of experimental medicine, 228(1), 69–74.
- Cramer, S. C. (2008). Repairing the human brain after stroke: I. Mechanisms of spontaneous recovery. Annals of neurology, 63(3), 272–287.
- Hellstrom, K., Lindmark, B., Wahlberg, B., & Fugl-Meyer, A. R. (2003). Self-efficacy in relation to impairments and activities of daily living disability in elderly patients with stroke: a prospective investigation. Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine, 35(5), 202–207.
- Hurkmans, H. L., Ribbers, G. M., Streur-Kranenburg, M. F., Stam, H. J., & van den Berg-Emons, R. J. (2011). Energy expenditure in chronic stroke patients playing Wii Sports: a pilot study. Journal of neuroengineering and rehabilitation, 8, 38.
- im, J. H., Jang, S. H., Kim, C. S., Jung, J. H., & You, J. H. (2009). Use of virtual reality to enhance balance and ambulation in chronic stroke: a double-blind, randomized controlled study. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists, 88(9), 693– 701.
- Kolominsky-Rabas, P. L. (2006). Lifetime Cost of Ischemic Stroke in Germany: Results and National Projections From a Population-Based Stroke Registry: The Erlangen Stroke Project. Stroke, 37(5), 1179–1183.
- Laver, K. E., George, S., Thomas, S., Deutsch, J. E., & Crotty, M. (2011). Virtual reality for stroke rehabilitation. Cochrane database of systematic reviews (Online), (9), CD008349.
- Sas, A. C., Wurm, S., & Scheidt-Nave, C. (2010). Alter und Gesundheit. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, 53(5), 404–416.
- Schaechter, J. D. (2004). Motor rehabilitation and brain plasticity after hemiparetic stroke. Progress in neurobiology, 73(1), 61–72.
- Vellas, B. J., Wayne, S. J., Romero, L. J., Baumgartner, R. N., & Garry, P. J. (1997). Fear of falling and restriction of mobility in elderly fallers. Age and ageing, 26(3), 189–193.
- Weerdesteyn, V., Niet, M. de, van Duijnhoven, H. J. R., & Geurts, A. C. H. (2008). Falls in individuals with stroke. The Journal of Rehabilitation Research and Development, 45(8), 1195.
- Yavuzer, G.,Eser, F., Karakus, D., Karaoglan, B., & Stam, H. J. (2006). The effects of balance training on gait late after stroke: a randomized controlled trial. Clinical Rehabilitation, 20(11), 960–969.
- Zhang, Y., Chapman, A.-M., Plested, M., Jackson, D., & Purroy, F. (2012). The Incidence, Prevalence, and Mortality of Stroke in France, Germany, Italy, Spain, the UK, and the US: A Literature Review. Stroke Research, 2012(7), 1–11.
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.