
THERAPY-Magazin
Less fear of falling!
A study shows that gait training with the THERA-Trainer e-go significantly improves balance and walking ability in patients with acquired brain injury—reducing fear of falling and enhancing confidence in daily life.

Jakob Tiebel
Health Business Consultant
Influence of robot-assisted gait training with the THERA‑Trainer e-go on self-experienced gait stability of patients with acquired brain damage.
Introduction
The top therapy goal of every person is to regain or maintain their unrestricted independence. An important element of independence is the ability to walk. Numerous studies have shown that restrictions in the ability to walk are a major concern in patients with neurogenic movement disorders. The physical activity of those affected is often greatly reduced, and balance is limited. This has negative effects on the various activities of daily life and on individual quality of life. This often results in a much higher fall risk. Those affected find themselves in a vicious circle of fear and avoidance behaviour.
A task-specific therapeutic approach has proven to be particularly effective for the re-learning of walking. Those affected need to practise the function of walking. And in as intense and sustained a way as possible. What is critical is training at the patient’s individual limit of performance. In the case of existing balance disorders, this includes walking in the multimodal setting (multiple tasks) with and without disturbances (perturbations). That way, confidence in one’s own abilities can be recovered. But how is this possible in the clinical-therapeutic setting, without provoking the risk of falling and manifesting existing fears in those affected?
The THERA‑Trainer e-go is a mobile gait trainer capable of practical therapy support. It is a mobile training device equipped with electric motors. During the therapy, the patient is secured to a supporting frame by a pelvic belt. The securing system has no influence at all on the upper body. However, the patient is completely protected against falls thanks to the pelvic belt safety device, so that controlled walking exercise on the level is possible without relieving body weight.
The device is controlled by the therapist via a wired control unit. A speed adjusted to the patient’s individual performance level can be selected via a stepless speed control system. It is also possible to force higher walking speeds and speed variations. Directional changes can be made from standing and in the forward movement. The THERA-Trainer e-go also has a two-stage adjustable balance release unit, which allows individual adaptation during exercise to the patient’s ability to balance.
The patient walks independently, which requires active displacement of the body’s centre of gravity. Even more extended walking distances, up to the limit of performance, are therefore possible without a risk of falling. The arms can swing reactively during walking. Even everyday activities such as carrying and transporting objects can be practised under realistic conditions. With soft floor mats and suitable tread surfaces which can be moved over using the THERA-Trainer e-go, it is possible to simulate various surfaces. This ensures that training is specific, task-oriented and relevant to everyday life. The patient’s self-activity is encouraged.
As of 2018, the THERA-Trainer e-go has already been used internationally in numerous rehabilitation facilities in gait therapy. However, to date there has been insufficient research into the influence of training on self-experienced gait stability and self-efficacy of patients with acquired brain damage.
The aim of the present study was to investigate the influence of robot-assisted gait training (RAGT) using the THERA-Trainer e-go on self-experienced gait stability and self-efficacy, as part of a post-market clinical follow-up evaluation.
The top therapy goal of every person is to regain or maintain their unrestricted independence. An important element of independence is the ability to walk. Numerous studies have shown that restrictions in the ability to walk are a major concern in patients with neurogenic movement disorders. The physical activity of those affected is often greatly reduced, and balance is limited. This has negative effects on the various activities of daily life and on individual quality of life. This often results in a much higher fall risk. Those affected find themselves in a vicious circle of fear and avoidance behaviour.
A task-specific therapeutic approach has proven to be particularly effective for the re-learning of walking. Those affected need to practise the function of walking. And in as intense and sustained a way as possible. What is critical is training at the patient’s individual limit of performance. In the case of existing balance disorders, this includes walking in the multimodal setting (multiple tasks) with and without disturbances (perturbations). That way, confidence in one’s own abilities can be recovered. But how is this possible in the clinical-therapeutic setting, without provoking the risk of falling and manifesting existing fears in those affected?
The THERA‑Trainer e-go is a mobile gait trainer capable of practical therapy support. It is a mobile training device equipped with electric motors. During the therapy, the patient is secured to a supporting frame by a pelvic belt. The securing system has no influence at all on the upper body. However, the patient is completely protected against falls thanks to the pelvic belt safety device, so that controlled walking exercise on the level is possible without relieving body weight.
The device is controlled by the therapist via a wired control unit. A speed adjusted to the patient’s individual performance level can be selected via a stepless speed control system. It is also possible to force higher walking speeds and speed variations. Directional changes can be made from standing and in the forward movement. The THERA-Trainer e-go also has a two-stage adjustable balance release unit, which allows individual adaptation during exercise to the patient’s ability to balance.
The patient walks independently, which requires active displacement of the body’s centre of gravity. Even more extended walking distances, up to the limit of performance, are therefore possible without a risk of falling. The arms can swing reactively during walking. Even everyday activities such as carrying and transporting objects can be practised under realistic conditions. With soft floor mats and suitable tread surfaces which can be moved over using the THERA-Trainer e-go, it is possible to simulate various surfaces. This ensures that training is specific, task-oriented and relevant to everyday life. The patient’s self-activity is encouraged.
As of 2018, the THERA-Trainer e-go has already been used internationally in numerous rehabilitation facilities in gait therapy. However, to date there has been insufficient research into the influence of training on self-experienced gait stability and self-efficacy of patients with acquired brain damage.
The aim of the present study was to investigate the influence of robot-assisted gait training (RAGT) using the THERA-Trainer e-go on self-experienced gait stability and self-efficacy, as part of a post-market clinical follow-up evaluation.
Methodology
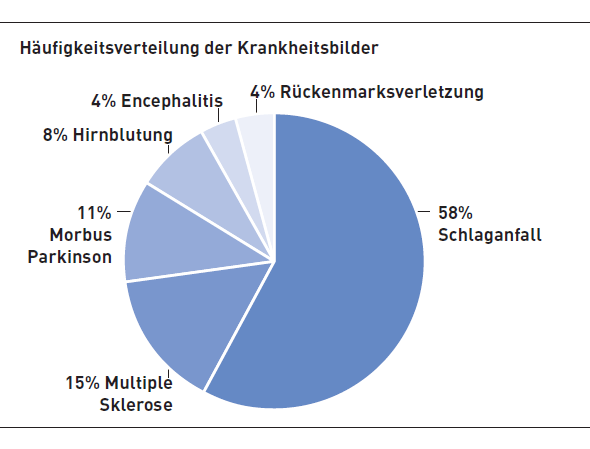
From several inpatient neurological rehabilitation facilities, a total of 26 patients with impaired mobility, age 65.3 (± 11.1), 15 strokes (58%), 4 multiple sclerosis (15%), 3 Parkinson’s disease (11%), 2 cerebral haemorrhage (8%), 1 encephalitis (4%), 1 spinal cord injury (4%) were recruited and included in the case series intervention study.
From several inpatient neurological rehabilitation facilities, a total of 26 patients with impaired mobility, age 65.3 (± 11.1), 15 strokes (58%), 4 multiple sclerosis (15%), 3 Parkinson’s disease (11%), 2 cerebral haemorrhage (8%), 1 encephalitis (4%), 1 spinal cord injury (4%) were recruited and included in the case series intervention study.
Inclusion criteria
- at least three-week hospital stay
- neurological disease with impaired walking ability
- cognitive requirements to participate in the therapy and testing procedures and to follow the instructions of the investigator
- interest and motivation to participate
- at least three-week hospital stay
- neurological disease with impaired walking ability
- cognitive requirements to participate in the therapy and testing procedures and to follow the instructions of the investigator
- interest and motivation to participate
Exclusion criteria
- lack of initial walking ability (FAC <2) or unrestricted ability to walk indoors and outdoors (FAC >4)
- health condition, not to be able to train in the submaximal range
- pain during therapy using the THERA‑Trainer e-go
- lack of initial walking ability (FAC <2) or unrestricted ability to walk indoors and outdoors (FAC >4)
- health condition, not to be able to train in the submaximal range
- pain during therapy using the THERA‑Trainer e-go
Intervention
As part of the rehabilitation program, the patients were given a 30-minute task-specific gait training with the THERA-Trainer e-go to complement conventional physiotherapy and ergotherapy (average 2.8 ± 1.6 training sessions per week) up to five days a week. The intervention period was 3 weeks.
As part of the rehabilitation program, the patients were given a 30-minute task-specific gait training with the THERA-Trainer e-go to complement conventional physiotherapy and ergotherapy (average 2.8 ± 1.6 training sessions per week) up to five days a week. The intervention period was 3 weeks.
Measurement variables
A key element was the collection of Patient Reported Outcomes (PROs) at the end of the intervention phase (T1). In addition, standardised motor assessments were performed at the beginning (T0) and at the end (T1).
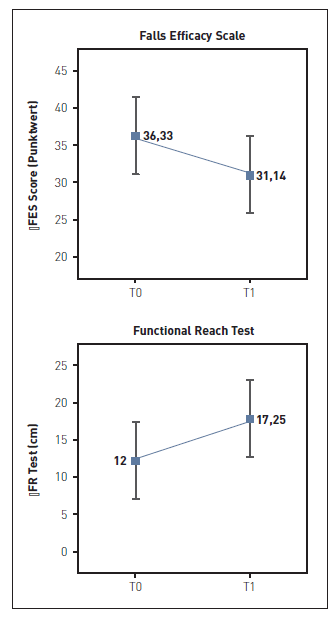
The individual fall risk of the patients was assessed by means of the Functional Reach Test (FR). The FR is a dynamic balance test that is easy to use in practice and uses a continuous score system. It measures in centimetres how far a patient with a secure stance can reach forward with an extended right arm. Patients with neurogenic movement disorders may lose their balance or even fall. The degree of uncertainty and the associated risk of falls can be derived from the measurement results.
Subjective gait stability or the fear of falling was recorded using the Falls Efficacy Scale (FES). Since fear is a latent variable that can not be directly operationalised, FES (based on question items) helps to record fall-associated self-efficacy in a standardised manner. The person to be measured estimates the individual competencies in successfully coping with certain actions associated with the risk of falling.
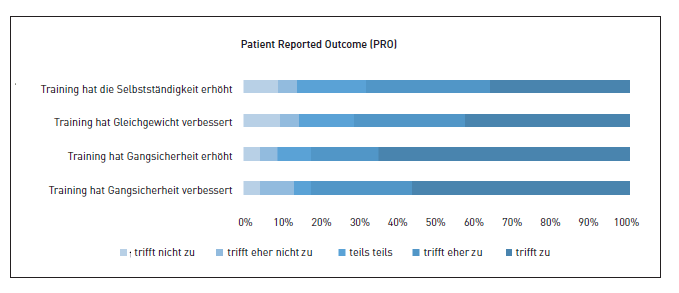
Recording the PROs was designed to investigate the patient’s perspective, which is not captured by the clinical measurement variables in that form, but is important to the patient and compliance with the therapy. Of course, treatments must be clinically and cost effective, but they should also deliver acceptable and desirable results for patients. Measures of clinical efficacy typically do not provide information about how a patient feels or works or what he or she believes is achieved through treatment. Measuring this element of acceptance requires patient-based evidence that includes measures of well-being. The PRO was recorded in four dimensions. At the end of the intervention period, patients were able to subjectively evaluate the influence of training on walking ability, gait stability, balance and their independence in everyday life on a five-point Likert scale (1 not true to 5 true).
A key element was the collection of Patient Reported Outcomes (PROs) at the end of the intervention phase (T1). In addition, standardised motor assessments were performed at the beginning (T0) and at the end (T1).
The individual fall risk of the patients was assessed by means of the Functional Reach Test (FR). The FR is a dynamic balance test that is easy to use in practice and uses a continuous score system. It measures in centimetres how far a patient with a secure stance can reach forward with an extended right arm. Patients with neurogenic movement disorders may lose their balance or even fall. The degree of uncertainty and the associated risk of falls can be derived from the measurement results.
Subjective gait stability or the fear of falling was recorded using the Falls Efficacy Scale (FES). Since fear is a latent variable that can not be directly operationalised, FES (based on question items) helps to record fall-associated self-efficacy in a standardised manner. The person to be measured estimates the individual competencies in successfully coping with certain actions associated with the risk of falling.
Recording the PROs was designed to investigate the patient’s perspective, which is not captured by the clinical measurement variables in that form, but is important to the patient and compliance with the therapy. Of course, treatments must be clinically and cost effective, but they should also deliver acceptable and desirable results for patients. Measures of clinical efficacy typically do not provide information about how a patient feels or works or what he or she believes is achieved through treatment. Measuring this element of acceptance requires patient-based evidence that includes measures of well-being. The PRO was recorded in four dimensions. At the end of the intervention period, patients were able to subjectively evaluate the influence of training on walking ability, gait stability, balance and their independence in everyday life on a five-point Likert scale (1 not true to 5 true).
Statistics
Data collection and descriptive statistics were performed using Microsoft Excel (version 16.14.1). The inferential statistical analysis was carried out using the statistics program JASP (Version 0.9.0.1).
The paired samples for variable walking speed, walking distance, FES and FR were evaluated non-parametrically using the Wilcoxon test for paired samples, because all test variables did not meet the requirements for the use of parametric test procedures. The significance level was set to α <0.05 on two sides.
Data collection and descriptive statistics were performed using Microsoft Excel (version 16.14.1). The inferential statistical analysis was carried out using the statistics program JASP (Version 0.9.0.1).
The paired samples for variable walking speed, walking distance, FES and FR were evaluated non-parametrically using the Wilcoxon test for paired samples, because all test variables did not meet the requirements for the use of parametric test procedures. The significance level was set to α <0.05 on two sides.
Results
A total of 26 patients, age 65.3 (± 11.1), were included in the evaluations. The data sets from a total of 209 training sessions were analysed. Each patient completed an average of 8.58 (95% CI: 6.05, 11.11) training sessions within the three-week intervention period.
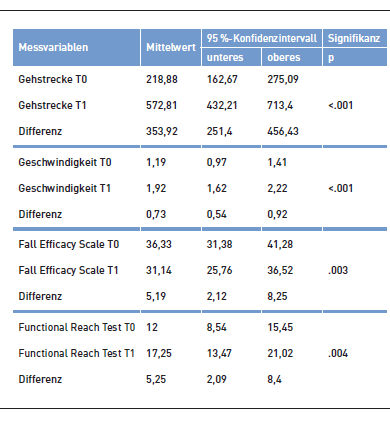
In the FR, patients improved their reach by an average of 5.25 cm (95% CI: 2.09, 8.4; p=.004). Fear of falling decreased by an average of 5.19 (95% CI 2.12, 8.25, p = .003) points on the FES.
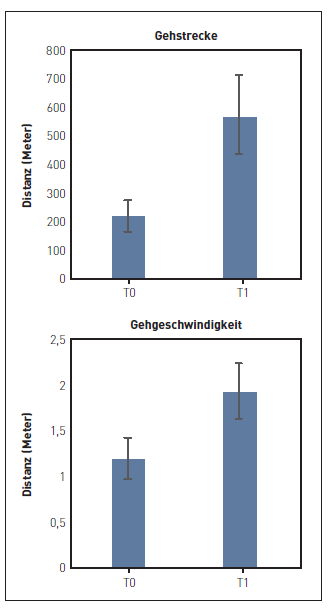
The pre-post analysis of the training data shows a significant increase in walking distance of 353.92 metres (95% CI: 251.4, 456.43; p=<.001) and in walking speed of 0.73 km/h (95% CI: 0.54, 0.92; p <0.001) in the course of therapy.
The PROs show that the training with the THERA-Trainer e-go had a positive influence on the ability to walk and gait stability from the perspective of the patients, and led to improvements in the area of balance and independence in everyday life.
A total of 26 patients, age 65.3 (± 11.1), were included in the evaluations. The data sets from a total of 209 training sessions were analysed. Each patient completed an average of 8.58 (95% CI: 6.05, 11.11) training sessions within the three-week intervention period.
In the FR, patients improved their reach by an average of 5.25 cm (95% CI: 2.09, 8.4; p=.004). Fear of falling decreased by an average of 5.19 (95% CI 2.12, 8.25, p = .003) points on the FES.
The pre-post analysis of the training data shows a significant increase in walking distance of 353.92 metres (95% CI: 251.4, 456.43; p=<.001) and in walking speed of 0.73 km/h (95% CI: 0.54, 0.92; p <0.001) in the course of therapy.
The PROs show that the training with the THERA-Trainer e-go had a positive influence on the ability to walk and gait stability from the perspective of the patients, and led to improvements in the area of balance and independence in everyday life.
Conclusion
The objective was to investigate the influence of robot-assisted gait training (RAGT) with the THERA-Trainer e-go on the self-experienced gait stability of patients with acquired brain damage. The evaluations show that the patients’ balance improved significantly and the fear of falling decreased significantly. More than 80% of patients attributed these improvements to the task-specific training with the THERA-Trainer e-go, amongst other things.
Gait training using the THERA-Trainer e-go therefore represents a practical addition to conventional gait therapy in neurological rehabilitation. Through training, patients experience an improvement in gait-specific parameters and benefit at the level of participation from increased self-efficacy.
The objective was to investigate the influence of robot-assisted gait training (RAGT) with the THERA-Trainer e-go on the self-experienced gait stability of patients with acquired brain damage. The evaluations show that the patients’ balance improved significantly and the fear of falling decreased significantly. More than 80% of patients attributed these improvements to the task-specific training with the THERA-Trainer e-go, amongst other things.
Gait training using the THERA-Trainer e-go therefore represents a practical addition to conventional gait therapy in neurological rehabilitation. Through training, patients experience an improvement in gait-specific parameters and benefit at the level of participation from increased self-efficacy.
Ambulante Rehabilitation
Fachkreise
Gait
Stationäre Rehabilitation
THERAPY 2019-I
THERAPY Magazine
Training zu Hause
Wohnen im Alter & Langzeitpflege

Jakob Tiebel
Health Business Consultant
Jakob Tiebel is OT and studied applied psychology with a focus on health economics. He has clinical expertise from his previous therapeutic work in neurorehabilitation. He conducts research and publishes on the theory-practice transfer in neurorehabilitation and is the owner of an agency for digital health marketing.
References:
- Duncan, P. W./Studenski, S./Chancler, J./Prescott B.: Functional reach: Predictive validity in a sample of elderly male veterans, in: Journal of Gerontology 47, 1992, 3, 93-98.
- Duncan, P. W./Weiner, D. K./Chancler, J./Studenski, S.: Functional reach: A new clinical measure of balance, in: Journal of Gerontology 45, 1990, 6, 192-197.
- Tiebel J. (2018): Intensive continuous therapy for paraplegia, THERAPY Magazine, 2(1), 38-41.
- Tiebel, J. (2018): Back to everyday life, step by step, THERAPY Magazine, 2(1), 42-43.
- Tiebel, J. (2018): Practice walking by walking, THERAPY Magazine, 2(1), 20-24.
- Tiebel, J. (2018): Putting hybrid gait trainers to the test, THERAPY Magazine, 2(1), 30-37.
- Yardley, L./Beyer, N./Hauer, K./Kempen, G./Piot-Ziegler, C./Todd, C. (2005): Development and initial validation of the Falls Efficacy Scale International (FES-I). Age and Ageing, 34(6), 614-619.
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.