THERAPY-Magazin
Therapeutic Gamification and rehabilitation technologies in use
Discover how MossRehab and MRRI leverage gamification, VR, and robotics like Lokomat, C-Mill, and THERA-Trainer lyra to enhance neurorehabilitation outcomes—both in clinic and at home.

Laurel J. Buxbaum
Deputy Director of the Moss Rehabilitation Research
Institute (MRRI) and Director of the MRRI Cognition and Action Laboratory and Professor of Rehabilitation Medicine
of Rehabilitation Medicine at Thomas Jefferson University.
How MossRehab and Moss Rehabilitation Research Institute (MRRI) are using Therapeutic Gaming and technology to Improve Recovery after neurological injuries
Rehabilitation is critical after a stroke or brain injury to improve an individual’s chances of regaining functional and cognitive abilities. Studies show that intensive therapy with highly repetitive and task-oriented practices offers the most benefits after neurological injuries. “After a stroke or brain injury, the neural pathways involved with the brain are interrupted,” explains Amanda Rabinowitz, PhD, institute scientist and director of the Brain Injury Neuropsychology Laboratory at the Moss Rehabilitation Research Institute (MRRI).
„Repetitive therapy exercises help to strengthen that pathway in the brain or develop a new one to restore function."
Maintaining patient interest and enthusiasm in traditional therapies over time is difficult. While therapists help engage patients in exercises, individuals often lose their drive in completing the same routines repeatedly. Therapeutic gaming provides the stimuli to keep patients engaged in rehab exercises with therapy equipment that features computer-based and/or virtual reality images. In addition, gaming therapy helps individuals to understand and visualize exercise goals.
“If somebody is working on their arms with a reaching exercise, therapy equipment with gamification can project an image, such as a fruit, to frame how to retrieve it,” Dr. Rabinowitz states. “Using this type of visualization helps patients to master the right movement for more natural motions. It would be hard to duplicate that motion by following a worksheet that outlines the exercise.”
Therapeutic gaming also provides immediate, robust feedback. Flashing lights and sounds triggered when a patient makes the correct movement encourages them to keep going. At the same time, therapists get information on patient progress to determine if they should level up or move to another activity.
“I use this extensively in occupational therapy to improve arm range of motion and cognitive skills,” remarks Stephanie Farm, MS, OTR/L, who works with adult and pediatric persons with brain injuries and serves as the occupational therapy team leader at the MossRehab Drucker Brain Injury Center. “The Myro has various fine motor attachments so patients can use a joystick to work on gross grasp skills, a pencil for writing activities, or a piece to promote grasp. Cognitive games also prompt patients to scan the screen and identify items that don’t belong or find missing components or use colors to complete a sequence.”
“If somebody is working on their arms with a reaching exercise, therapy equipment with gamification can project an image, such as a fruit, to frame how to retrieve it,” Dr. Rabinowitz states. “Using this type of visualization helps patients to master the right movement for more natural motions. It would be hard to duplicate that motion by following a worksheet that outlines the exercise.”
Therapeutic gaming also provides immediate, robust feedback. Flashing lights and sounds triggered when a patient makes the correct movement encourages them to keep going. At the same time, therapists get information on patient progress to determine if they should level up or move to another activity.
“I use this extensively in occupational therapy to improve arm range of motion and cognitive skills,” remarks Stephanie Farm, MS, OTR/L, who works with adult and pediatric persons with brain injuries and serves as the occupational therapy team leader at the MossRehab Drucker Brain Injury Center. “The Myro has various fine motor attachments so patients can use a joystick to work on gross grasp skills, a pencil for writing activities, or a piece to promote grasp. Cognitive games also prompt patients to scan the screen and identify items that don’t belong or find missing components or use colors to complete a sequence.”
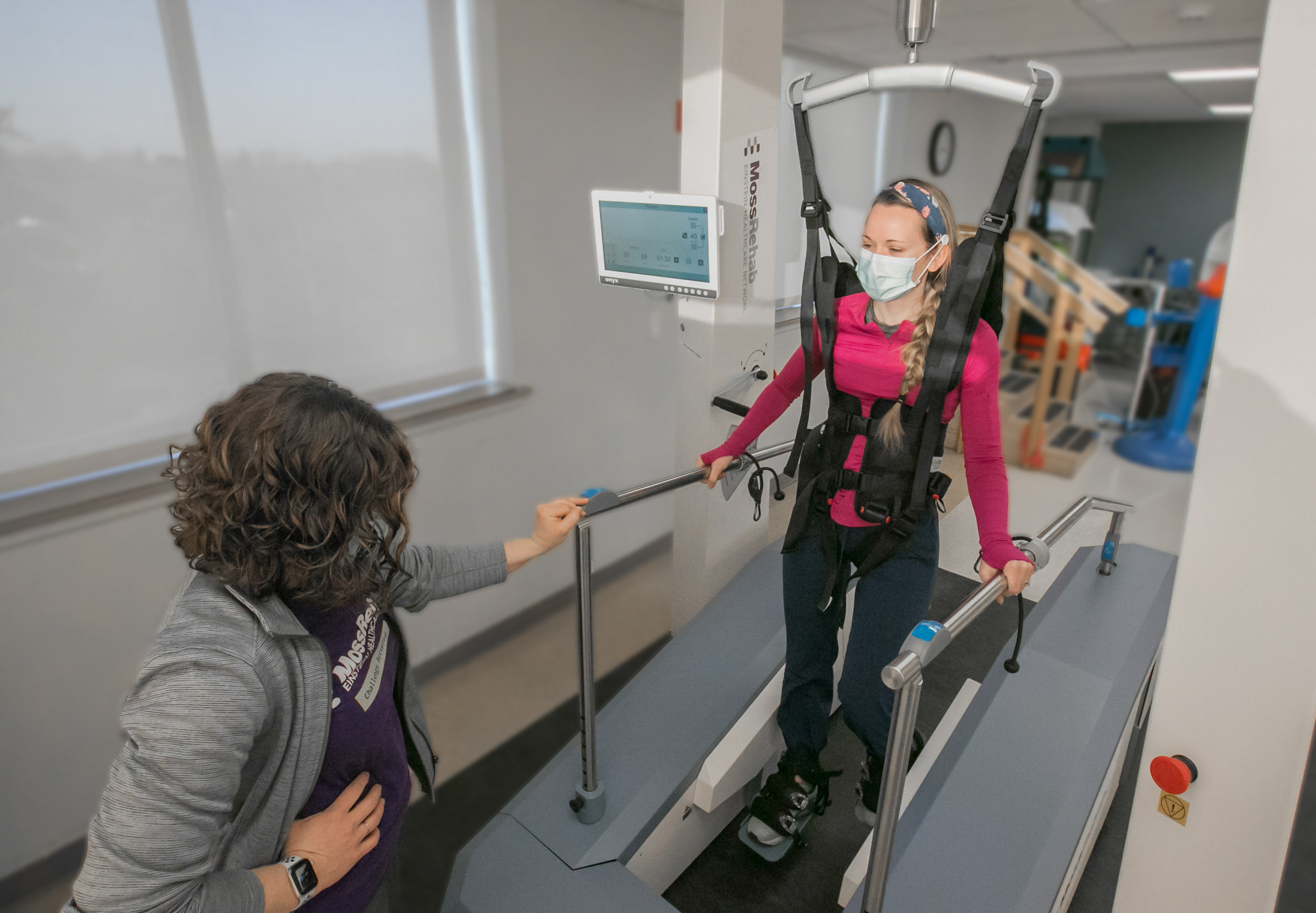
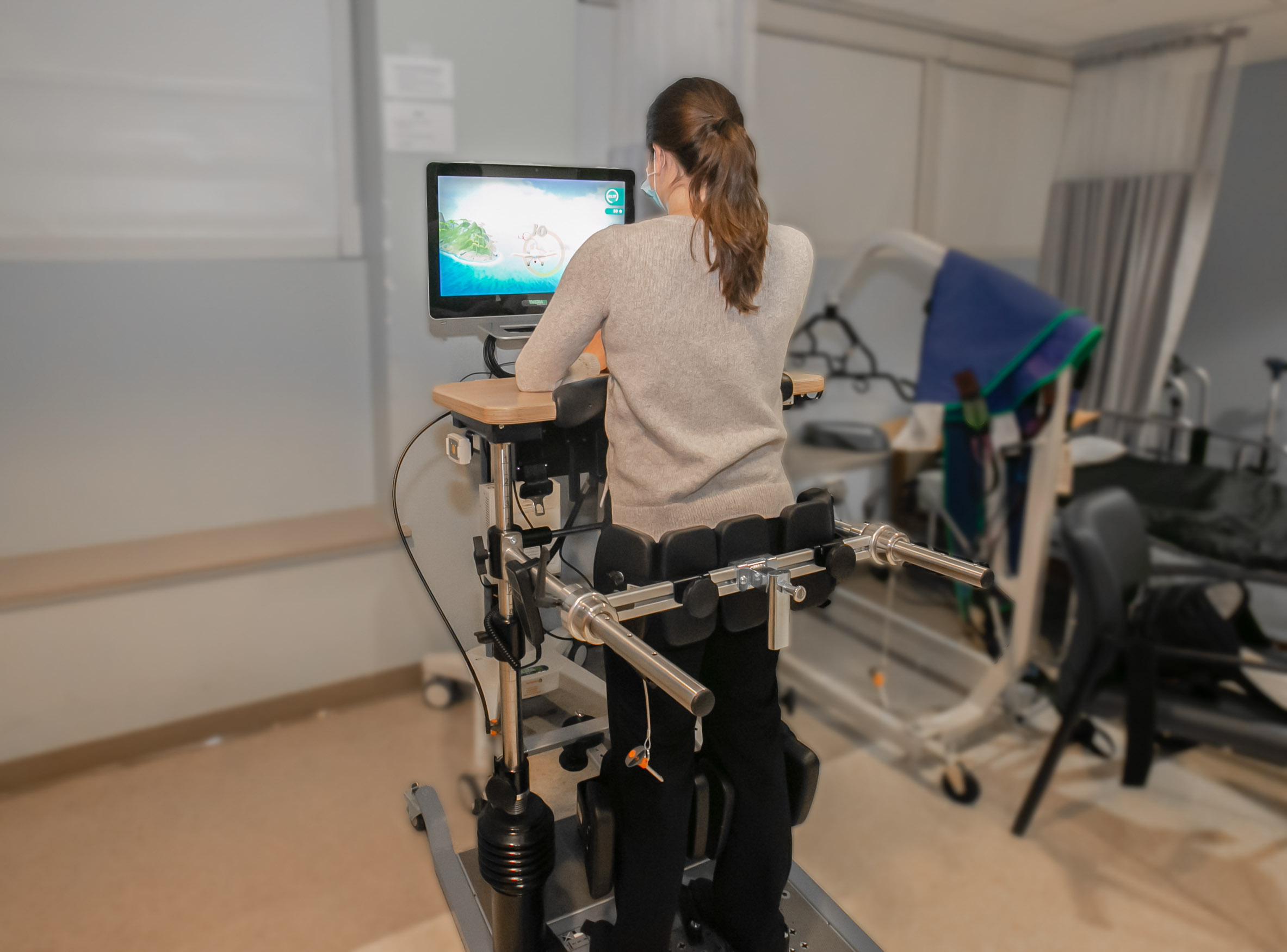
Gaming therapy for gait rehabilitation
MossRehab is the only rehab facility with two Lokomat devices, a THERA-Trainer lyra and a G-EO at one site that offers robot-assisted gait therapy for patients who experienced neurological injuries. For the Lokomat, the patient is supported by a harness above the treadmill, while an exoskeleton assists the legs to improve walking. Various game-like exercises help patients to meet their goals. MossRehab also recently added the C-Mill, a high-tech treadmill that features a large LCD screen and an overhead projector for gait rehabilitation. The C-Mill device offers augmented and virtual reality games that replicate real-life activities to prepare patients for the outside world.
“One application requires a patient standing at an intersection of two crossing roads to lift their leg if a car approaches from the right or left to avoid it,” says Matthew Vnenchak, PT, MS, NCS. “The high-tech treadmill gives visual and auditory feedback if a patient successfully or unsuccessfully completes the task for immediate feedback and reinforcement.”
MossRehab is the only rehab facility with two Lokomat devices, a THERA-Trainer lyra and a G-EO at one site that offers robot-assisted gait therapy for patients who experienced neurological injuries. For the Lokomat, the patient is supported by a harness above the treadmill, while an exoskeleton assists the legs to improve walking. Various game-like exercises help patients to meet their goals. MossRehab also recently added the C-Mill, a high-tech treadmill that features a large LCD screen and an overhead projector for gait rehabilitation. The C-Mill device offers augmented and virtual reality games that replicate real-life activities to prepare patients for the outside world.
“One application requires a patient standing at an intersection of two crossing roads to lift their leg if a car approaches from the right or left to avoid it,” says Matthew Vnenchak, PT, MS, NCS. “The high-tech treadmill gives visual and auditory feedback if a patient successfully or unsuccessfully completes the task for immediate feedback and reinforcement.”
Researching the future
MossRehab continues to evaluate new technologies and conduct research to develop new therapeutic gaming technology. One study led by Dylan Edwards, PhD, Director of MRRI and the Human Motor Recovery Laboratory, is testing a new therapeutic gaming system for motor recovery after a stroke that uses immersive digital gaming to create an environment in which patients control a dolphin swimming through the water. The engaging exercises will help people with impaired arm function to improve their recovery.
Another study using virtual reality gamification focuses on reducing phantom limb pain. Laurel Buxbaum, PsyD, Associate Director of MRRI and Director of the Cognition and Action Laboratory, is working on a virtual reality treatment based on the theory of providing alternative feedback to the brain in the form of a visual image of a missing limb to eliminate a sensory mismatch to reduce pain.
Wearing a VR headset, patients with limb amputations will perform a series of activities such as scooting around a maze on a virtual chair while kicking down barricades and typing on a virtual keyboard with the legs to surf the Internet. The VR system fills in an image of the missing limb so that amputees see themselves complete. “Visualizing and moving limbs simultaneously provides a corrective signal to the brain that reduces phantom limb pain,” explains Dr. Buxbaum.
MossRehab continues to evaluate new technologies and conduct research to develop new therapeutic gaming technology. One study led by Dylan Edwards, PhD, Director of MRRI and the Human Motor Recovery Laboratory, is testing a new therapeutic gaming system for motor recovery after a stroke that uses immersive digital gaming to create an environment in which patients control a dolphin swimming through the water. The engaging exercises will help people with impaired arm function to improve their recovery.
Another study using virtual reality gamification focuses on reducing phantom limb pain. Laurel Buxbaum, PsyD, Associate Director of MRRI and Director of the Cognition and Action Laboratory, is working on a virtual reality treatment based on the theory of providing alternative feedback to the brain in the form of a visual image of a missing limb to eliminate a sensory mismatch to reduce pain.
Wearing a VR headset, patients with limb amputations will perform a series of activities such as scooting around a maze on a virtual chair while kicking down barricades and typing on a virtual keyboard with the legs to surf the Internet. The VR system fills in an image of the missing limb so that amputees see themselves complete. “Visualizing and moving limbs simultaneously provides a corrective signal to the brain that reduces phantom limb pain,” explains Dr. Buxbaum.
Creating VR patient assessments
Dr. Bauxbaum also developed a Virtual Reality Lateralized Attention Test (VR-LAT) that assesses the severity of a stroke on attention, visual search, and multi-tasking. Typically, pencil and paper tests diagnose this problem where patients bisect lines or cross out specific items in a listing. However, these tests are not sensitive enough to detect subtle deficits and are not strong predictors of performance in the real world.
The VR-LAT creates a virtual environment where individuals travel a path while naming trees and statues of animals and ignoring auditory distractions. Using test results, clinicians can assess spatial neglect and the disposition to visual and auditory distraction to determine patient safety in navigating environments. The assessment also provides a baseline measurement for therapy.
The Virtual Reality Non-Use Test (VR-NU) is another assessment tool developed by Dr. Bauxbaum team that uses gaming theory to evaluate arm function after a stroke. Wearing a VR head-mounted display equipped with headphones and motion tracking sensors affixed to the wrists, patients reach for objects on different virtual shelves. The VR-NU test tracks accuracy, trajectory, response time in the completion of tasks under different conditions. The ten-minute assessment tool will help clinicians determine the severity of arm limitations after stroke.
Dr. Bauxbaum also developed a Virtual Reality Lateralized Attention Test (VR-LAT) that assesses the severity of a stroke on attention, visual search, and multi-tasking. Typically, pencil and paper tests diagnose this problem where patients bisect lines or cross out specific items in a listing. However, these tests are not sensitive enough to detect subtle deficits and are not strong predictors of performance in the real world.
The VR-LAT creates a virtual environment where individuals travel a path while naming trees and statues of animals and ignoring auditory distractions. Using test results, clinicians can assess spatial neglect and the disposition to visual and auditory distraction to determine patient safety in navigating environments. The assessment also provides a baseline measurement for therapy.
The Virtual Reality Non-Use Test (VR-NU) is another assessment tool developed by Dr. Bauxbaum team that uses gaming theory to evaluate arm function after a stroke. Wearing a VR head-mounted display equipped with headphones and motion tracking sensors affixed to the wrists, patients reach for objects on different virtual shelves. The VR-NU test tracks accuracy, trajectory, response time in the completion of tasks under different conditions. The ten-minute assessment tool will help clinicians determine the severity of arm limitations after stroke.
„There is a great deal of technology available to assist with patient mobilization in a way that is safer for both the patient and clinician. One of the challenges with technology is how to keep the patient engaged for the entire time the equipment is being utilized to allow for increased intensity and frequency of use. The THERA-soft software used in conjunction with the Balo makes it fun and interesting for patients when we are working on dynamic standing balance tasks. THERA-soft can be tailored to the patient‘s specific needs so they can easily appreciate gains being made“
Home therapies
Home-based therapy devices help those having transportation or resource challenges or needing to supplement outpatient rehabilitation. That’s the premise behind a portable gaming console for homes use that assists patients in recovering upper extremity functions after a stroke. Dr. Edwards was a principal investigator for a pivotal trial of the home-based therapy equipment that features arcade like computer-based and cognitive games.
Dr. Rabinowitz is working with a Rehabilitation Engineering Resource Center (RERC) on developing mobile rehabilitation interventions and therapies for home-based use in persons with TBI. Currently, she is leading the development of a chatbot for personalized interactions with patients to track activities, plans, and goals between therapy sessions, all via text message. Designed to support outpatient brain injury treatment, the chatbot provides encouraging messages, activity updates, and other feedback to help patients meet therapy goals.
Another research program is evaluating feedback received from sensor-based neurorehabilitation devices offered by FlintRehab to determine how people use different gamification features during therapy. Findings will enable developers to design more effective and engaging applications. In addition, Dr. Rabinowitz is working to integrate home-based rehab devices (one is a sensorized glove worn while performing hand and finger exercises to music) with an application called PT Pal to create a platform that collects data and identifies trends to monitor and track patient progress between clinical visits.
With the help of MRRI researchers, MossRehab remains on the pulse of therapeutic gaming in research and developing new innovative technologies for both clinical and home-based use. Our goal is to provide patients and therapists with the best tools and clinical programs to boost the effectiveness of rehabilitation in achieving long-term recovery goals.
For more information using robotics-assisted rehabilitation solutions to assess and treat neurological deficits, visit www.mossrehab.com/technology.
Home-based therapy devices help those having transportation or resource challenges or needing to supplement outpatient rehabilitation. That’s the premise behind a portable gaming console for homes use that assists patients in recovering upper extremity functions after a stroke. Dr. Edwards was a principal investigator for a pivotal trial of the home-based therapy equipment that features arcade like computer-based and cognitive games.
Dr. Rabinowitz is working with a Rehabilitation Engineering Resource Center (RERC) on developing mobile rehabilitation interventions and therapies for home-based use in persons with TBI. Currently, she is leading the development of a chatbot for personalized interactions with patients to track activities, plans, and goals between therapy sessions, all via text message. Designed to support outpatient brain injury treatment, the chatbot provides encouraging messages, activity updates, and other feedback to help patients meet therapy goals.
Another research program is evaluating feedback received from sensor-based neurorehabilitation devices offered by FlintRehab to determine how people use different gamification features during therapy. Findings will enable developers to design more effective and engaging applications. In addition, Dr. Rabinowitz is working to integrate home-based rehab devices (one is a sensorized glove worn while performing hand and finger exercises to music) with an application called PT Pal to create a platform that collects data and identifies trends to monitor and track patient progress between clinical visits.
With the help of MRRI researchers, MossRehab remains on the pulse of therapeutic gaming in research and developing new innovative technologies for both clinical and home-based use. Our goal is to provide patients and therapists with the best tools and clinical programs to boost the effectiveness of rehabilitation in achieving long-term recovery goals.
For more information using robotics-assisted rehabilitation solutions to assess and treat neurological deficits, visit www.mossrehab.com/technology.
balo
Fachkreise
Gait
lyra
Science
Standing & Balancing
Stationäre Rehabilitation
THERAPY 2022-I
THERAPY Magazine

Laurel J. Buxbaum
Deputy Director of the Moss Rehabilitation Research
Institute (MRRI) and Director of the MRRI Cognition and Action Laboratory and Professor of Rehabilitation Medicine
of Rehabilitation Medicine at Thomas Jefferson University.
Laurel J. Buxbaum, PsyD, is the Deputy Director of the Moss Rehabilitation Research Institute (MRRI) and Director of the MRRI Laboratory for Cognition and Action, as well as a Professor of Rehabilitation Medicine at Thomas Jefferson University. She has authored over 100 peer-reviewed articles and book chapters and has served as an associate editor for the journals Cognition, Cortex, and Journal of Neuropsychology. She has received grants from the National Institute of Health, the National Institute of Disability and Rehabilitation Research, and the James S. McDonnell Foundation. Dr. Buxbaum has received numerous awards, including the Arthur Benton Mid-Career Award from the International Neuropsychological Society, the Widener University Graduate Award for Excellence in Professional Psychology, the Viste Award from the American Society of Neurorehabilitation, and the Freda Newcombe Prize from the British Neuropsychological Society. Her lab focuses on researching the representation of complex actions in the brain, the influence of action representations on knowledge about manipulable objects, the relationships between action and language processing, visual neglect, and phantom pain phenomena in individuals with amputations. Her work encompasses a translational "pipeline" from basic cognitive neuroscience to neurorehabilitation.

Dylan J. Edwards
Director of the Moss Rehabilitation Research Institute (MRRI) and Director of the MRRI Laboratory for Motor Rehabilitation. He is also Professor of Neuroscience and Director of the
of the Neuroscience and Robotics Laboratory at Edith Cowan University
Dylan J. Edwards, PhD, is the Director of the Moss Rehabilitation Research Institute (MRRI) and Director of the MRRI Laboratory for Motor Rehabilitation, with the goal of understanding motor symptoms and motor recovery to develop rehabilitation treatment strategies. He is also a Professor of Neuroscience and Director of the Laboratory for Neuroscience and Robotics at Edith Cowan University. The lab engages in multiple research lines focused on restoring functional movement in individuals following neurological damage from stroke, spinal cord injuries, or other neurological conditions. He earned his PhD in Neurophysiology at the Center for Neuromuscular and Neurological Disorders at the University of Western Australia (now Perron Institute for Neurological and Translational Sciences). Before joining MRRI in 2018, Dr. Edwards was Director of the Laboratory for Non-invasive Brain Stimulation at the Burke Neurological Institute and Lecturer in Clinical Neurophysiology at Weill Cornell Medicine in New York. During his time in New York, he led a long-standing collaboration between Harvard Medical School, the Massachusetts Institute of Technology in Boston, and the Burke-Cornell Neurological Institute in New York, bridging technology, neurology, and rehabilitation medicine. This interdisciplinary collaboration resulted in over a decade of extramural funding for studies on human motor rehabilitation. Dr. Edwards is internationally recognized as a leader in the field of neurorehabilitation, with his work leading to scientific advances in predicting rehabilitation outcomes, non-invasive brain stimulation techniques, and rehabilitation robotics, both in methodology and application.

Amanda Rabinowitz
Institute Scientist and Director of the Brain Injury,
Neuropsychology Laboratory at the Moss Rehabilitation Research Institute (MRRI), Research Assistant Professor
of Rehabilitation Medicine at Thomas Jefferson University, Director of the Moss Traumatic Brain Injury (TBI) Model System
Amanda Rabinowitz, PhD, is a Research Scientist and Director of the Brain Injury Neuropsychology Laboratory at the Moss Rehabilitation Research Institute (MRRI), as well as an Assistant Professor of Rehabilitation Medicine at Thomas Jefferson University. Additionally, Dr. Rabinowitz leads the Moss Traumatic Brain Injury (TBI) Model System, a world-class center of excellence that provides cutting-edge research, innovative treatments, and valuable programs for individuals with traumatic brain injuries, continuously funded since 1997. As a neuropsychologist, Dr. Rabinowitz investigates the outcomes of chronic brain injuries across the spectrum of traumatic brain injury severity. Her work particularly focuses on psychosocial factors that confer resilience after a brain injury, with a particular interest in self-regulation as a key mechanism. Several of Dr. Rabinowitz’s projects utilize mobile technology to enhance the assessment and intervention of brain injuries. She collaborates with local and national partners on studies of long-term outcomes of brain injuries. Dr. Rabinowitz has authored or co-authored over 100 publications in academic journals and is internationally recognized as an expert in neuropsychology of traumatic brain injuries. Dr. Rabinowitz earned her BA in Cognitive Neuroscience and Psychology from the University of Pennsylvania and her MS and PhD in Clinical Psychology from Pennsylvania State University. During her studies, she completed her internship in neuropsychology at the Warren Alpert Medical School of Brown University. Prior to establishing her research lab at MRRI, Dr. Rabinowitz completed a postdoctoral fellowship at the University of Pennsylvania.
References:
Related contents
Find related exciting contents in our media library.
Mehr laden
This is not what you are searching for? Knowledge
Meet our specialists.
Are you interested in our solutions? Schedule a meeting with a Consultant to talk through your strategy and understand how TEHRA-Trainer can help you to advance rehabilitation.
You need to load content from reCAPTCHA to submit the form. Please note that doing so will share data with third-party providers.
More InformationYou are currently viewing a placeholder content from Turnstile. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More Information